|
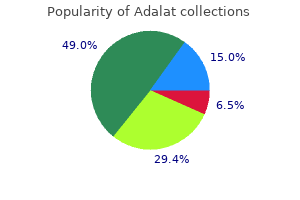
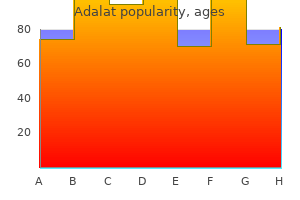
Adalat dosages: 30 mg, 20 mg
Adalat packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
Adalat 30 mg purchase fast deliveryAlthough primarily a motor nerve supplying mylohyoid and the anterior belly of the digastric blood pressure printable chart buy adalat 20 mg visa, the mylohyoid nerve carries some sensory fibres that will enter the mandible via a quantity of small retromental foramina in the neighborhood of the genial tubercles to supply some sensation to the anterior enamel blood pressure during pregnancy discount 30 mg adalat overnight delivery. Although the deep temporal nerves are primarily motor arteria heel buy 30 mg adalat amex, it has been suggested that terminal branches might move from the substance of tem poralis to enter the mandible by way of foramina within the retromolar region to supply some sensation to molar enamel blood pressure very low purchase adalat 20 mg online. In the cervical plexus, the great auricular nerve, formed by the anter ior primary rami of the second and third cervical spinal nerves, provides skin over the angle of the mandible (p. It is possible that this nerve could present a branch that penetrates the mandible to provide a quantity of of the cheek enamel. It is subsequently not considered an applicable land mark for inferior alveolar nerve block (Ezoddini Ardakani et al 2010). The lingual nerve passes throughout the floor of the periosteum lin gually to the lower wisdom tooth, separated from the tooth solely by a cortical plate of bone no thicker than an eggshell. Damage to this nerve results in altered sensation (paraesthesia) to the ipsilateral facet of the tongue and floor of mouth. Indeed, surgical treatment could only necessitate the elimination of the crown, leaving behind the roots (after appropriate root filling). Max illary third molars are only not often impacted because they erupt postero inferiorly. A clear radiograph is required before any tooth extraction is undertaken to find a way to alert the dental surgeon to any issues that could be encountered. For instance, although the inferior alveolar nerve and its accompanying vessels usually lie beneath the roots of the third permanent molar within the mandibular canal, the neurovascular bundle might occupy the next position, near the roots, and should even run between the roots. In this situation, the inferior alveolar nerve is in danger during extraction of third molars; harm to the nerve might result in paraesthesia in the distribution of the psychological nerve, with consequent altered sensation or numbness within the decrease lip. The root of a mandibu lar premolar could sometimes be unusually lengthy and may be in close relationship to the mental nerve, which can then be in danger throughout extraction of this tooth. If the tooth is totally lined by bone and mucosa, it is rather unlikely to cause any signs, and the topic stays unaware of its presence until the tooth is seen on a routine dental radiograph. The creating cyst could displace the tooth because it expands and the tooth could find yourself as far-off as the condylar neck or coronoid process. More generally, the erupting knowledge tooth erupts partially before impacting in opposition to the distal facet of the second molar. When this occurs, signs are widespread due to recurrent soft tissue inflamma tion and an infection across the partially erupted tooth brought on by food impaction. This situation is called pericoronitis and, if the infecting organism is virulent, the an infection may quickly unfold into the adjacent tissue spaces as described elsewhere. The tooth only deserves surgical removal if the affected person suffers a extreme bout or multiple bouts of peri coronitis. These injec tions can either be performed transorally � posterior superior alveolar nerve block, maxillary nerve block, inferior alveolar nerve block, lingual nerve block and mandibular nerve block � or, extra not often, by an exter nal route by way of the skin of the face � maxillary nerve block, inferior alveolar nerve block and mandibular nerve block. In the case of the mandible, the anterior tooth can be anaesthetized by easy diffusion methods, because the bone is relatively skinny. In this case, the inferior alveolar nerve has to be anaesthe tized before it enters the inferior alveolar canal. The needle has to be positioned inside the pterygomandibular space to obtain a profitable in ferior alveolar nerve block. The lingual nerve can be normally blocked, because it lies close to the inferior alveolar nerve. Any harm to blood vessels in the infratemporal fossa � generally, the pterygoid venous plexus � can result in haematoma formation. In excessive cases, bleeding can track via the inferior orbital fissure, leading to a retrobulbar haematoma, which can lead to loss of visible acuity or blindness. Intravascular injection of native anaesthetic resolution (which often contains adrenaline (epinephrine)) can have profound systemic results, and for this reason an aspirating syringe is all the time used to verify that the needle has not entered a vessel previous to injection (vessels in this space that theoretically could additionally be entered embrace the maxil lary and inner carotid arteries). If the needle is placed too medially, it may enter medial pterygoid; if directed too laterally, it could penetrate temporalis. If the needle is positioned too deeply, anaesthetic solution might cause a quick lived facial nerve palsy because of loss of conduction from the facial nerve in the area of the parotid gland. Local anaesthetic answer could enter the orbit by way of the inferior orbital fissure and provides orbital symptoms, the most probably being a brief lived paralysis of the abducens nerve with lack of exercise of lateral rectus. The root apices of the maxillary cheek tooth are close to, and will even invaginate, the maxillary sinus. The permanent tooth most com monly concerned is the second molar, adopted by the primary molar; less incessantly, premolars and the third molar may be concerned. The likeli hood of cavitation of the maxillary sinus will increase considerably after tooth extraction. B, Cone beam computed tomography of the same affected person shown in A; the image within the sagittal airplane clearly shows the 2 buccal root apices (arrow) of the everlasting maxillary second molar tooth invaginating into the maxillary sinus (M). It consists of a bigger superficial and a smaller deep part, con tinuous with one another across the posterior border of mylohyoid. The sympathetic root is derived from the plexus on the facial artery and consists of postganglionic fibres from the superior cervical ganglion that traverse the submandibular ganglion with out synapsing. These fibres are vasomotor to the blood vessels of the submandibular and sublingual glands. Below, it often overlaps the intermediate tendon of digastric and the insertion of stylohyoid. This part of the submandibular gland presents inferior, lateral and medial surfaces, and is partially enclosed between two layers of deep cervical fascia that reach from the higher cornu of the hyoid bone. The superficial layer is hooked up to the decrease border of the man dible and covers the inferior floor of the gland. The deep layer is connected to the mylohyoid line on the medial surface of the mandible and covers the medial floor of the gland. The inferior floor, lined by pores and skin, platysma and deep fascia, is crossed by the facial vein and the cervical branch of the facial nerve. Near the mandible, the submandibular lymph nodes are involved with the gland and a few may be embedded inside it. The lateral floor is related to the submandibular fossa on the medial floor of the body of the mandible and the mandibular connect ment of medial pterygoid. The facial artery grooves its posterosuperior part, lies at first deep to the gland and then emerges between its lateral surface and the mandibular attachment of the medial pterygoid to attain the lower border of the mandible. Below, the medial floor is expounded to the stylohyoid muscle and the posterior belly of digastric. Submandibular duct the submandibular duct is about 5 cm lengthy and has a thinner wall than the parotid duct. It begins from quite a few tributaries in the superficial part of the gland and emerges from the medial surface of this part of the gland behind the posterior border of mylohyoid. It traverses the deep a part of the gland, and then passes at first up and slightly again for about 5 mm, this sharp bend over the free fringe of mylohyoid being generally identified as the genu of the duct. As the duct traverses the deep a part of the gland, it receives small tributaries draining this part of the gland. It has been instructed beforehand that the genu of the duct predisposes to the stasis of saliva and thereby encourages salivary stone (sialolith) formation, but this is somewhat controversial and largely unproven. The anterior finish of the contralateral sublingual gland lies in entrance, and the deep part of the submandibular gland lies behind. The mandible above the anterior a part of the mylohyoid line, the sub lingual fossa, is lateral, and genioglossus is medial, separated from the gland by the lingual nerve and submandibular duct. Deep a half of the submandibular gland the deep part of the gland extends forwards to the posterior end of the sublingual gland. Vascular supply, innervation and lymphatic drainage the arterial supply is from the sublingual branch of the lingual artery and the submental department of the facial artery. Vascular supply and lymphatic drainage the arteries supplying the gland are branches of the facial and lingual arteries. The lymph vessels drain into the deep cervical group of lymph nodes (particularly the juguloomohyoid node), interrupted by the sub mandibular nodes. Innervation the secretomotor provide to the submandibular gland is derived from the submandibular ganglion. Submandibular ganglion this small, fusiform physique is a peripheral parasympathetic ganglion.
Buy generic adalat 30 mg on lineThe sensory fibres that cross via the ciliary ganglion are derived from the nasociliary nerve arrhythmia quiz ecg trusted adalat 20 mg. They enter the brief ciliary nerves and carry sensation from the cornea blood pressure medication vision problems adalat 30 mg generic without prescription, the ciliary body and the iris blood pressure normal 30 mg adalat purchase with mastercard. The margin medial to the papilla lacks eyelashes and forms the lacrimal part of the eyelid blood pressure medication used to treat anxiety adalat 30 mg buy on-line. When wanting straight ahead, the upper eyelid overlaps the upper part of the cornea by 2�3 mm, whereas the lower lid margin lies just under the corneoscleral junction (limbus). When the eyelids are closed, the higher lid strikes right down to cowl the entire of the cornea. Entropion describes the inversion of the eyelid with corresponding inturning of the eyelashes (trichiasis), which contact the cornea and trigger irritation. This corresponds to the placement of the ciliary (marginal) a half of orbicularis oculi and is an important surgical landmark, since an incision at this point allows the eyelid to be cut up into anterior and posterior lamellae along a comparatively bloodless airplane. The eyelashes lie in entrance of the grey line, and the circular openings of the tarsal glands (Meibomian glands) lie behind it. The tarsal glands are often visible by way of the palpebral conjunctiva, when the eyelids are everted, as a collection of parallel, faint yellow strains arranged perpendicular to the lid margins. The eyelids pass to adjoining facial pores and skin without apparent demarcation, though their limits are clearly defined in pathological situations such as oedema. A distinguished superior palpebral furrow or fold lies roughly opposite the higher margin of the tarsal plate and is deeply recessed when the lids are open. Asians have a pores and skin flap, the epicanthus, which begins laterally in the superior palpebral fold and progresses medially to cowl the medial canthus. Infant Caucasians incessantly have a transient epicanthus, which sometimes persists in the adult. A less outstanding inferior palpebral furrow occupies an identical place in the pores and skin of the decrease lid and deepens on downward gaze. A nasojugal furrow extends obliquely from the medial decrease margin of the bony orbit to the cheek, and a malar furrow could additionally be seen laterally along the inferior orbital rim in center age, but solely sometimes and faintly in the young. Orbital branches of the pterygopalatine ganglion Several rami orbitales come up dorsally from the pterygopalatine ganglion and enter the orbit via the inferior orbital fissure. There is robust experimental proof from research of animals, together with monkeys, that postganglionic parasympathetic branches move directly to the lacrimal gland, ophthalmic artery and choroid. By their reflex closure, achieved by contraction of orbicularis oculi, they shield the attention from injury and protect the eyes from extreme gentle. Periodic blinking maintains a thin movie of tears over the cornea that prevents desiccation; movement of the eyelids during blinking helps ensure the even distribution of the tear film and facilitates tear outflow via the nasolacrimal drainage system. The upper eyelid is larger and extra cell than the lower eyelid and incorporates an elevator muscle, levator palpebrae superioris (see above). A transverse opening, the palpebral fissure, lies between the free margins of the lids, which be a part of at their extremities (termed the medial and lateral canthus). The medial canthus is roughly 2 mm decrease than the lateral canthus; this distance is elevated in some Asiatic groups. It is separated from the eyeball by a small triangular area, the lacrimal lake (lacus lacrimalis), during which a small, reddish body referred to as the lacrimal caruncle is situated. A small elevation, the lacrimal papilla, is positioned on each palpebral margin approximately one-sixth of the best way along from the medial canthus of the eye. There is a small aperture, the punctum lacrimale, within the centre of the papilla that forms the opening to the lacrimal drainage system. The skin is extremely skinny and is steady at the palpebral margins with the conjunctiva. The subcutaneous connective tissue may be very delicate, seldom incorporates any adipose tissue, and lacks elastic fibres. The palpebral a part of orbicularis oculi is subdivided anatomically into ciliary, pretarsal and preseptal components. The palpebral fibre bundles are skinny and pale, and lie parallel with the palpebral margins. The major nerves lie in the submuscular layer, which implies that local anaesthetics must be injected deep to orbicularis oculi. Each is convex and conforms to the configuration of the anterior floor of the attention. The superior tarsus, the bigger of the two, is semi-oval, approximately 10 mm in height centrally. The smaller inferior tarsus is narrower and roughly 4 mm in vertical peak. Key: 1, pupil; 2, plica semilunaris; 3, lacrimal caruncle; four, medial canthus; 5, conjunctiva; 6, upper eyelid; 7, eyelashes; 8, lateral canthus; 9, lid margin; 10, iris; 11, lower eyelid. At delivery, the higher eyelid is at its lowest place and the margin of the decrease eyelid is close to the centre of the pupil. Between the ages of 3 and 6 months, the higher eyelid reaches its maximum peak after which declines in a linear style. The distance between the centre of the pupil and the margin of the decrease eyelid increases linearly until the age of 18 months, when it stabilizes in place. The most typical pattern of the lower eyelid crease is a single crease at birth and a double crease by the age of about three years. Ageing mainly affects the scale of the horizontal eyelid fissure, which lengthens by about 10% between the ages of 12 and 25, and shortens by nearly the same quantity between center age and old age. The peak stage of progress within the horizontal dimension of the palpebral fissure is reached between the ages of 17 and 19 years, in the vertical dimension between 10 and 13 years, and within the intercanthal distance between 14 and 16 years in Asian kids (Park et al 2008). It splits at its insertion into the tarsal plates to surround the lacrimal canaliculi, and lies in entrance of the nasolacrimal sac and the orbital septum. It passes from the lateral ends of the tarsal plates to a small tubercle on the zygomatic bone throughout the orbital margin and is extra deeply situated than the medial palpebral ligament. It lies beneath the orbital septum and the lateral palpebral raphe of orbicularis oculi. The deepest fibres of the aponeurosis of levator palpebrae superioris are hooked up to the anterior surface of the superior tarsus. The superior and inferior tarsal plates are additionally related to a thin lamina of smooth muscle forming the superior and inferior tarsal muscle tissue, respectively. The muscle is innervated by the sympathetic nervous system and, on contraction, elevates the eyelid. A corresponding but much less outstanding inferior tarsal muscle in the decrease eyelid unites the inferior border, and possibly also the anterior floor, of the inferior tarsus to the capsulopalpebral fascia, which is the anterior growth of the fused fascial sheath of inferior rectus and inferior oblique. Contraction of inferior rectus throughout downward gaze therefore also pulls the lower lid downwards. Palpebral glands Tarsal (Meibomian) glands are modified sebaceous glands embedded in the tarsi. They are yellow and arranged in roughly 25 parallel rows perpendicular to the eyelid margin in the higher lid, and slightly fewer in the lower lid. They occupy the total tarsal peak and are due to this fact longer centrally the place the tarsi are higher. Each gland consists of a straight tube with many lateral secretory diverticula, and opens by a minute orifice on the free palpebral margin. It is enclosed by a basement membrane, and is lined at its orifice by stratified epithelium and elsewhere by a single layer of polyhedral cells. The sebaceous secretion of the tarsal glands spreads over the margins of the eyelids, and so an oily layer is drawn over the tear movie because the palpebral fissure opens after a blink, decreasing evaporation and contributing to tear movie stability. The presence of the oily, hydrophobic secretions of tarsal glands alongside the margins of the eyelids also inhibits the spillage of tears on to the face. Obstruction of the tarsal gland ducts by lipid and cellular debris might end in lipogranulomatous inflammation and the scientific manifestations of an inside hordeolum or chalazion. Their branches course laterally alongside the tarsal edges to type superior and inferior arcades (two in the upper eyelid and one in the lower). The eyelids are additionally supplied by branches of the infraorbital, facial, transverse facial and superficial temporal arteries. The veins that drain the eyelids are bigger and extra numerous than the arteries; they move both superficially to veins on the face and brow, or deeply to the ophthalmic veins throughout the orbit.
Adalat 30 mg purchaseThey begin at the posteroinferior aspect of the cavernous sinus and run back in the petroclival fissure arrhythmia hereditary best 30 mg adalat, a groove between the petrous temporal and basilar occipital bones blood pressure medication lack of energy 30 mg adalat generic visa. On each side arteria vitellina purchase 30 mg adalat otc, the inferior petrosal sinus subsequent passes via the anteromedial a part of the jugular foramen arrhythmia update 2015 purchase 30 mg adalat overnight delivery, accompanied by a meningeal branch of the ascending pharyngeal artery, and descends obliquely backwards to drain into the superior jugular bulb. It typically drains through a vein in the hypoglossal canal to the suboccipital vertebral plexus. Each receives labyrinthine veins through the cochlear canaliculus and the vestibular aqueduct, and tributaries from the medulla oblongata, pons and inferior cerebellar surface. The venous spaces within the sphenopetroclival area, which are stuffed anteriorly by blood from the cavernous sinus, medially by blood from the basilar plexus, and laterally by blood from the superior petrosal sinus, usually drain into the inferior petrosal sinuses (Iaconetta et al 2003). The cavity of the cavernous sinus is formed when the two layers of dura that cover the anterior side of the pituitary gland separate from each other on the lateral margin of the sella; the outer (endosteal) layer continues laterally to form the anterior (or sphenoidal) wall of the cavernous sinus, whereas the inner (meningeal) layer stays connected to the pituitary gland and runs back towards the dorsum sellae to form the medial (or sellar) wall of the cavernous sinus. The posterior dural wall is positioned behind the dorsum sellae and upper clivus, and is shared with the basilar plexus. Each sinus contains the cavernous section of the interior carotid artery, related to a perivascular sympathetic plexus. The cavernous carotid artery has a number of portions, from proximal to distal: short ascending, posterior genu, horizontal, anterior genu. The anterior genu of the cavernous carotid artery continues as the paraclinoidal phase of the carotid artery, which generally protrudes into the sphenoidal sinus cavity. The meningohypophysial trunk arises sometimes from the posterior genu and provides off the inferior hypophysial, tentorial and dorsal meningeal arteries. The inferolateral trunk arises a number of millimetres distal to the meningohypophysial and distributes across the nerves on the lateral wall of the sinus. The oculomotor and trochlear nerves and the ophthalmic division of the trigeminal nerve all lie in the lateral wall of the sinus. Several major venous spaces can been recognized inside the sinus in relation to the cavernous carotid artery: superior, posterior, inferior and lateral (modified from Harris and Rhoton 1976). The superior and inferior ophthalmic veins drain into the inferior house; the basilar plexus and inferior petrosal sinus drain into the posterior area; the superior petrosal sinus opens into the superior area; and the superficial middle cerebral vein, inferior cerebral veins and sphenoparietal sinus could drain into the lateral compartment. Veins traversing the emissary sphenoidal foramen, foramen ovale and foramen lacerum may also drain into the cavernous sinus. Less regularly, the central retinal vein and frontal tributary of the center meningeal vein additionally drain into it. The dura has been eliminated on the right half of the specimen to present the roof of the cavernous sinus (oculomotor triangle), and the maxillary and mandibular nerves running on the ground of the center fossa. B, the ophthalmic nerve has been retracted inferiorly to show the inside of the cavernous sinus (abducens nerve, inside carotid artery and its branches) via the infratrochlear triangle. Tumours can come up throughout the cavernous sinus (meningiomas, haemangiomas, schwannomas) or prolong into the cavernous sinus from adjacent areas (typically, pituitary adenomas that invade the medial wall of the sinus). Transcranial microsurgical approaches enter the cavernous sinus through the lateral wall (infratrochlear triangle) or roof (oculomotor triangle) of the sinus. Recently launched endoscopic endonasal approaches facilitate access to the cavernous sinus from its anterior (sphenoidal) and medial (sellar) partitions. This is a important medical emergency with a high danger of disseminated cerebritis and cerebral venous thrombosis. The traditional signs are ptosis, proptosis (which may be pulsatile), chemosis, periorbital oedema, and extraocular dysmotility causing diplopia secondary to a mix of third, fourth and sixth cranial nerve palsies. Hypo- or hyperaesthesia of the ophthalmic divisions of the fifth cranial nerve and a decreased corneal reflex may also be detected. The superior and posterior intercavernous sinuses lie in the anterior and posterior hooked up borders of the diaphragma sellae and they thus kind a complete circular venous sinus. The inferior intercavernous sinuses are irregular and plexiform in nature, and commonly encountered in a surgical transnasal strategy to the pituitary gland. Obliteration of any intercavernous sinus has no medical consequences as a end result of all connections are valveless and the direction of move in them is reversible. The basilar venous plexus interconnects the cavernous sinuses and inferior and superior petrosal sinuses, and joins the internal vertebral venous plexus. Each sinus curves medially to open into the anterior part of the cavernous sinus, and receives small veins from the adjoining dura mater and generally the frontal ramus of the middle meningeal vein. Each may also receive connecting rami, in its center course, from the superficial middle cerebral vein, temporal lobe veins and the Meninges anterior temporal diploic vein. When these connections are properly developed, the sphenoparietal sinus is a large channel. In the posterior fossa, the dura is supplied by the meningeal branches of the occipital artery (one enters the cranium by the jugular foramen and another by the mastoid foramen), the posterior meningeal branches of the vertebral artery, occasional small branches of the ascending pharyngeal artery, which enter by the jugular foramen and hypoglossal canal, and the dorsal meningeal and tentorial arteries arising from the meningohypophysial trunk. The anatomy of the meningeal arteries explains the vascular supply for tumours arising from the meninges (meningiomas) and the architecture of dural arteriovenous fistulae and malformations. It commences close to the foramen magnum in several small channels, one joining the end of the sigmoid sinus, and connects with the internal vertebral plexuses. Marginal sinus Middle meningeal artery the marginal sinus encircles the foramen magnum. It communicates anteriorly with the basilar plexus and with the occipital sinus posteriorly. It sometimes drains to the sigmoid sinus or jugular bulb by small sinuses and should join extracranially to the internal vertebral venous plexus or the paravertebral or deep cervical veins within the suboccipital area. Emissary veins traverse cranial apertures and make connections between intracranial venous sinuses and extracranial veins. These connections are of medical significance in determining the spread of infection from extracranial foci to venous sinuses. They are additionally necessary because they might provide various drainage pathways in cases of venous sinus thrombosis. A mastoid emissary vein within the mastoid foramen connects the sigmoid sinus with the posterior auricular or occipital veins. A parietal emissary vein within the parietal foramen connects the superior sagittal sinus with the veins of the scalp. The venous plexus of the hypoglossal canal, which is occasionally a single vein, connects the sigmoid sinus and the internal jugular vein. A supracondylar emissary vein connects the sigmoid sinus and veins within the suboccipital triangle via the posterior condylar canal. A plexus of emissary veins (venous plexus of foramen ovale) connects the cavernous sinus to the pterygoid plexus through the foramen ovale. Two or three small veins traverse the foramen lacerum and connect the cavernous sinus and the pharyngeal veins and pterygoid plexus. A vein in the emissary sphenoidal foramen (of Vesalius) connects the cavernous sinus with the pharyngeal veins and pterygoid plexus.
[newline]The inside carotid venous plexus, which passes by way of the carotid canal, connects the cavernous sinus and the internal jugular vein. The petrosquamous sinus is an emissary vein that courses over the lateral superior surface of the petrous part of the temporal bone. It arises from the dorsolateral portion of the transverse sinus, earlier than its confluence with the superior petrosal sinus, and drains anteroinferiorly into the retromandibular vein and anteromedially into the pterygoid venous plexus. It normally disappears through the improvement of grownup venous patterns within the last three months of prenatal life. A vein may traverse the foramen caecum and join nasal veins with the superior sagittal sinus. An occipital emissary vein often connects the confluence of sinuses with the occipital vein by way of the occipital protuberance, and likewise receives the occipital diploic vein. The occipital sinus connects with variably developed veins around the foramen magnum (so-called marginal sinuses) and thus with the vertebral venous plexuses; this pathway supplies another venous drainage when the jugular vein is blocked or tied. The ophthalmic veins are probably emissary because they join intracranial to extracranial veins. Accessory meningeal artery the accent meningeal artery might come up from the maxillary or the middle meningeal artery. It enters the cranial cavity by way of the foramen ovale, and provides the trigeminal ganglion, dura mater and bone. Its primary distribution is extracranial, principally to medial pterygoid, lateral pterygoid (upper head), tensor veli palatini, the higher wing and pterygoid processes of the sphenoid bone, the mandibular nerve and otic ganglion.
Adalat 30 mg cheapEach sphenoidal concha has a centre arteria y arteriola discount adalat 20 mg fast delivery, showing superoposteriorly within the nasal capsule in the fifth month in utero hypertension 4011 buy discount adalat 30 mg. As this enlarges blood pressure percentile buy adalat 20 mg online, it partly surrounds a posterosuperior expansion of the nasal cavity hypertension 30s adalat 20 mg buy low price, which turns into the sphenoidal sinus. The posterior conchal wall is absorbed and the sinus invades the presphenoidal part. In the fourth 12 months, the concha fuses with the ethmoidal labyrinth and, before puberty, it fuses with the sphenoid and palatine bones. Postsphenoidal part the first centres seem in the larger wings at about the eighth week of fetal life, one within the basal cartilage of each wing below the foramen rotundum. These centres solely contribute to the foundation of the higher wing (near the foramen rotundum and pterygoid canal). The remainder of the greater wing and the lateral pterygoid plate are ossified in mesenchyme. At concerning the fourth month of fetal life, two centres appear, flanking the sella turcica, and shortly fuse. The hamulus is chondrified in the course of the third fetal month and at once begins to ossify. During the fourth month, a centre seems for every lingula, quickly becoming a member of the body. Postnatal particulars Presphenoidal and postsphenoidal elements fuse at about the eighth month in utero however an unciform cartilage persists after delivery in decrease components of the junction. At birth, the bone is tripartite and consists of a central part (body and lesser wings) and two lateral components (each consisting of a greater wing and pterygoid process). During the primary year, the greater wings and body unite around the pterygoid canals, and the lesser wings prolong medially above the anterior a part of the body, meeting to form the graceful, elevated jugum sphenoidale. An occasional vascular foramen, often erroneously termed the craniopharyngeal canal, is often seen within the anterior part of the hypophysial fossa. Anteriorly, the upper external floor shows an inconstant faint median ridge indicating the location of the fused symphysis menti. Inferiorly, this ridge divides to enclose a triangular psychological protuberance; its base is centrally depressed however raised on all sides as a psychological tubercle. The mental foramen, from which the psychological neurovascular bundle emerges, lies under either the interval between the premolar teeth, or the second premolar tooth, midway between the upper and lower borders of the physique. The posterior border of the foramen is easy and accommodates the nerve as it emerges posterolaterally. A faint exterior oblique line ascends backwards from each psychological tubercle, and sweeps below the psychological foramen; it turns into more marked as it continues into the anterior border of the ramus. The decrease border of the physique, the bottom, extends posterolaterally from the mandibular symphysis into the lower border of the ramus behind the third molar tooth. Behind the fossa, the base is thick and rounded: it has a slight anteroposterior convexity that adjustments to a gentle concavity because the ramus is approached, and so the base has an total sinuous profile. The upper border, the alveolar half, contains 16 alveoli for the roots of the lower teeth. It consists of buccal and lingual plates of bone joined by interdental and inter-radicular septa. Near the second and third molar tooth, the external oblique line is superimposed on the buccal plate. As within the maxilla, the shape and depth of the tooth sockets is related to the morphology of the roots of the mandibular tooth. The sockets of the incisor, canine and premolar teeth normally comprise a single root, while these for the three molar enamel each include two or three roots. It could also be impacted vertically, horizontally, mesially or distally, and its roots could additionally be bulbous, hooked, divergent or convergent, and sometimes embrace the mandibular (inferior dental) canal. The inside floor of the mandible is divided by an oblique mylohyoid line that gives attachment to mylohyoid (and, above its posterior end, to the superior pharyngeal constrictor, some retromolar fascicles of buccinator, and the pterygomandibular raphe behind the third molar). The mylohyoid groove extends downwards and forwards from the ramus under the posterior a part of the mylohyoid line and contains the mylohyoid neurovascular bundle. The space beneath the line is a slightly concave submandibular fossa and is related to the submandibular gland. The superior concave surface of each forms the anterior wall and part of the ground of a sphenoidal sinus. In situ, each has vertical quadrilateral anterior and horizontal triangular posterior elements. The anterior part consists of a superolateral depressed area, which completes the posterior ethmoidal sinuses and joins beneath with the orbital process of a palatine bone, and a smooth and triangular inferomedial space, which forms part of the nasal roof and is perforated above by the round opening connecting the sphenoidal sinus and spheno-ethmoidal recess. Anterior elements of the 2 bones meet within the midline, and protrude as the sphenoidal crest. The horizontal half appears in the nasal roof and completes the sphenopalatine foramen. Its medial edge articulates with the podium of the sphenoid and the ala of the vomer. Its apex, directed posteriorly, is superomedial to the vaginal strategy of the medial pterygoid plate and joins the posterior part of the ala. A small conchal part typically seems within the medial wall of the orbit, mendacity between the orbital plate of the ethmoid in entrance, the orbital strategy of the palatine bone under and the frontal bone above. It is readily identified by palpating the tip of the styloid course of and with mild blunt finger dissection passing anteriorly and medially to the pterygoid hamulus on the lower border of the medial pterygoid plate. Key: 1, pterygoid hamulus; 2, styloid course of; 3, foramen spinosum; four, foramen ovale; 5, lateral pterygoid plate. In an edentulous topic, it might be necessary to cut back any ridge-like prominence of the mylohyoid line to ensure that dentures to fit without traumatizing the overlying oral mucosa. Above the anterior ends of the mylohyoid lines, the posterior symphysial facet bears a small elevation, typically divided into higher and decrease parts, the mental spines (genial tubercles). The spines are sometimes fused to form a single eminence, or they could be absent, during which case their position is indicated merely by an irregularity of the floor. Midline lingual (genial) foramina, above and/or below the genial tubercles, and lateral lingual foramina within the premolar region are present in most mandibles and are of significance in the vascular provide to the symphysis. Appreciation of the three-dimensional course of the mandibular canal during its passage through the mandible from the mandibular to the psychological foramina is essential if damage to the inferior alveolar nerve is to be averted in third molar surgery, mandibular osteotomies, dental implant surgical procedure and harvesting of mandibular bone grafts. Coronoid course of the coronoid process projects upwards and slightly forwards as a triangular plate of bone. Its posterior border bounds the mandibular incisure, and its anterior border continues into that of the ramus. The lateral surface is comparatively featureless and bears the (external) oblique ridge in its decrease part. The mandibular foramen, via which the inferior alveolar neurovascular bundle passes to achieve access to the mandibular canal (see below), is sited halfway between the anterior and posterior borders of the ramus about degree with the occlusal surfaces of the enamel. It is overlapped anteromedially by a thin, sharp, triangular backbone, the lingula, to which the sphenomandibular ligament is hooked up, and which is also the landmark for an inferior alveolar local anaesthetic block injection. Below and behind the foramen, the mylohyoid groove runs obliquely downwards and forwards. The inferior border is steady with the mandibular base and meets the posterior border on the angle, which is typically everted in males however regularly inverted in females. The skinny superior border bounds the mandibular incisure (sigmoid or mandibular notch, incisura semilunaris), which is surmounted in front by the considerably triangular, flat coronoid process and behind by the condylar course of. The thick, rounded posterior border extends from the condyle to the angle, and is gently convex backwards above and concave below. The temporal crest is a ridge that descends on the medial aspect of the coronoid process from its tip to the bone just behind the third molar tooth. The triangular melancholy between the temporal crest and the anterior border of the ramus is the retromolar fossa (retromolar trigone). The ramus and its processes present attachment for the 4 main muscle tissue of mastication. Masseter is connected to the lateral surface, medial pterygoid is hooked up to the medial floor, temporalis is inserted into the coronoid course of and lateral pterygoid is hooked up to the condyle. The thickness of the ramus decreases markedly behind the exterior oblique line laterally, the temporal crest medially, and above the lingula; there may be fusion of the lateral and medial cortical plates. This is of importance in mandibular ramus osteotomies and in addition influences the frequency of fractures of the mandibular angle. When viewed from above, the condyle is roughly ovoid in outline, its anteroposterior dimension (approximately 1 cm) being roughly half its mediolateral dimension. The long axis of the condyle is at right angles to the mandibular ramus but, due to the flare of the ramus, the lateral pole of the condyle is barely anterior to the medial; if the long axes of the 2 condyles are prolonged, they meet at an obtuse angle, varying from 145� to 160�, on the anterior border of the foramen magnum.
20 mg adalat with visaThe blood provide to these muscles is from the sublingual branch of the lingual artery and the submental branch of the facial artery blood pressure chart normal buy adalat 30 mg. A department of the submental artery could anastomose with the mental artery blood pressure 300 over 200 buy 20 mg adalat with visa, permitting retrograde vascular provide to the body and symphysis (relevant in mandibular fractures) excel blood pressure chart 30 mg adalat order with mastercard. The vascular provide to the mandibular symphysis is of importance in dental implant surgery heart attack zippo cheap adalat 20 mg visa. The ramus, including the mandibular angle, is provided by the inferior alveolar artery and from the vessels supplying masseter and medial pterygoid. These differences produce a progressive improve in the incongruity of the alveolar processes of the jaws. There is full loss of the alveolar process, extending into the underlying basal bone. The psychological foramen (narrow arrows) and the mandibular canal (broad arrows) are on the superior border. Composition of the blood supply in the sublingual and submandibular spaces and its relationship to the lateral lingual foramen of the mandible. The posterior wall is fashioned by the tympanic plate, which also varieties the anterior wall of the external acoustic meatus. The anterior articular area of the fossa (articular fossa) is fashioned entirely from the squamous portion of the temporal bone and lined by articular tissue that extends anteriorly beyond the articular summit on to the preglenoid plane. The squamotympanic fissure marks the junction with the posterior non-articular (tympanic) space. The tegmen tympani, a bony plate of the petrous temporal, intervenes within the medial aspect of the fissure, the place the squamotympanic fissure turns into the petrotympanic fissure. The postglenoid tubercle on the root of the zygomatic arch, just anterior to the squamotympanic fissure, separates the squamotympanic fissure laterally from the tympanic plate. The condylar head, tilted forwards on the neck at an angle of approximately 30� (physiological anteversion), articulates with the fossa on its anterior and superior surfaces. Like the eminence, each its slope and form are variable, influenced by age, perform and dentition. In the coronal airplane, its shape varies from that of a gable (particularly marked in these whose food plan is hard) to roughly horizontal (in the edentulous). It might be unimaginable to measure the strain developed on the articular surfaces of the human jaw joint when biting; however, direct measurement of loads throughout the joint in animals has demonstrated important intermittent loading during mastication. There can additionally be irrefutable theoretical proof based mostly on Newtonian mechanics that the jaw joint is a weight-bearing joint. With a vertical bite drive of 500 N on the left first molar, the right condyle must support a load of well over 300 N (Osborn 1995). The non-working condyle is extra loaded than the condyle on the working side, which may help clarify why patients with a fractured condyle select to chew on the facet of the fracture. No gold normal exists as to what constitutes cervical fascia; nonetheless, the landmark paper by Grodinsky and Holyoke (1938) is typically recommended as a useful preliminary point of reference. The masticator space is closed posteriorly by the attachment of the deep cervical fascia, medial pterygoid and masseter (pterygomasseteric sling), and anteriorly, lateral to the ramus, by the agency attachment of masseter (the submasseteric space is a possible space). The masticator area is closed superiorly by both the temporal fascia laterally and the firm attachment of temporalis to the bone of the temporal fossa (the deep temporal space can additionally be solely a potential space). Medial to the ramus of the mandible, the pterygomandibular house (part of the masticator space) communicates freely with the pterygopalatine fossa, providing little resistance to the unfold of infection or tumours. Posteriorly penetrating maxillary tumours instantly contain the masticator space/infratemporal fossa and the pterygopalatine fossa. Above the level of the zygomatic arch, the temporal fascia provides each the superior and lateral limits, by its attachments to the superior temporal line and the zygomatic arch, respectively. Below the zygomatic arch, the investing layer of deep cervical fascia (superficial layer of deep cervical fascia) splits into two laminae to enclose masseter, the lower a part of temporalis and medial pterygoid, further defining the boundaries of the masticator house. The superficial (lateral) lamina covers masseter and attaches to the zygomatic arch, and the deep (medial) lamina runs on the deep surface of medial pterygoid, attaching to the cranium base medial to the foramen ovale (Guidera et al 2014). This fascial covering of the masticatory muscles is felt to be distinct from the parotid fascia (capsule). The contents of the masticator space are temporalis, masseter, medial and lateral pterygoid, the ramus and coronoid strategy of the mandible, the mandibular nerve and otic ganglion, the maxillary artery and the pterygoid venous plexus, and part of the buccal fat pad anterolaterally. The submasseteric, pterygomandibular, superficial and deep temporal areas are contained inside. The superficial temporal house lies between the temporal fascia laterally and temporalis medially. It lies between temporalis laterally and the temporal fossa of the cranium medially. Both spaces are in communication with the remainder of the masticator house inferiorly. There is debate as to the higher restrict of the masticator space, with the suggestion that it ought to be at the stage of the zygomatic arch. Since each temporal areas talk with the rest of the masticator house, a single masticator area incorporating the temporal fascia, muscle tissue and temporal areas is favoured (Guidera et al 2014). Thus the articular disc is attached individually to the temporal bone and to the mandibular condyle, forming what might be thought of two joint capsules. Longer fibres joining the condyle directly to the temporal bone may be thought to be reinforcing. The capsule is connected above to the anterior edge of the preglenoid plane, posteriorly to the lips of the squamotympanic fissure, between these to the perimeters of the articular fossa, and beneath to the periphery of the neck of the mandible. It extends downwards and backwards at an angle of roughly 45� to the horizontal, to attach to the lateral surface and posterior border of the neck of the condyle, deep to the parotid gland. A quick, virtually horizontal, band of collagen connects the articular tubercle in entrance to the lateral pole of the condyle behind. It could perform to forestall posterior displacement of the resting condyle and likewise initiates translation of the condyle on mouth opening. It is unusual in that its articular surfaces are lined by fibrocartilage, rather than hyaline cartilage; fibrocartilage is less susceptible to degeneration and has a higher restore capacity. This transverse ridge of dense bone, tilted down at an angle of roughly 25� to the occlusal plane, forms many of the articular floor of the mandibular fossa. It is strongly convex within the sagittal plane with a slight concavity in the coronal plane. It is a flat, thin band that descends from the spine of the sphenoid and widens as it reaches the lingula of the mandibular foramen; it has a median width at its insertion into the mandible of about 12 mm. Some fibres traverse the medial finish of the petrotympanic fissure and attach to the anterior malleolar course of. Foramina on the stage of, or above, the genial tubercle (superior genial foramen) and beneath the genial tubercle (inferior genial foramen) are almost all the time discovered (McDonnel et al 1994, Jacobs et al 2007). Lateral lingual foramina are usually identified, with a median distance above the decrease border of the mandible of 5 mm (Romanos et al 2012). The inferior foramen could include a department of the sublingual or submental arteries and a department of the mylohyoid nerve. The lateral foramen might include a department of the submental artery (Jacobs et al 2007, Nakajima et al 2014). Although the relative contributions from the individual vessels vary, anastomoses between these perforating vessels and the inferior alveolar artery, within the mandible, are common. The soft tissues in the anterior flooring of the mouth adjacent to the mandible are equipped by contributions from the sublingual, submental and mylohyoid arteries; there are considerable anastomoses between them (Romanos et al 2012, Nakajima et al 2014, Loukas et al 2008, Flanagan 2003). The exact source of the haemorrhage could be tough to detect and should come up from both inside the mandible and the delicate tissues within the ground of the mouth, from any of the above-named vessels. The anastomoses between the vessels might result in haemorrhage on both sides of mylohyoid and thus into the sublingual and the submental/submandibular areas bilaterally. As the lateral and midline lingual foramina are closer to the decrease border of the mandible, warning with longer implants has been beneficial in this region. Excessive bleeding in the floor of the mouth after endosseous implant placement: a report of two instances. The synovium is most ample within the bilaminar zone of the articular disc, forming unfastened folds posteriorly when the condyle is positioned in the glenoid fossa.
Syndromes - Weakness
- Palpitations (sensation of the heart beating)
- Avoid injuring the skin
- BUN
- Blood loss
- Back pain
- Growth may have slowed or stopped
Cheap adalat 30 mg overnight deliveryIn contrast heart attack telugu movie review buy generic adalat 30 mg online, darkish cells are wedge-shaped and have a narrow base blood pressure phobia order adalat 30 mg, few apical microvilli and dense pulse pressure decrease generic adalat 30 mg on line, fibrillar cytoplasm blood pressure medication list by class cheap adalat 30 mg mastercard. The endolymphatic sac has essential roles in the maintenance of vestibular perform. Endolymph produced elsewhere in the labyrinth is absorbed in this area, most likely mainly by the sunshine cells. Damage to the sac, or blockage of its connection to the remainder of the labyrinth, causes endolymph to accumulate; this produces hydrops, which impacts each vestibular and cochlear function. The epithelium can be permeable to leukocytes, together with macrophages, which may remove mobile debris from the endolymph, and to various cells of the immune system that contribute antibodies to this fluid. The osseous spiral lamina projects for part of the distance between the modiolus and the outer wall of the cochlea and is attached to the inside fringe of the basilar membrane. The endosteum of the outer wall is thickened to type a spiral cochlear ligament that tasks inwards as a triangular basilar crest hooked up to the outer rim of the basilar membrane. Immediately above this can be a concavity, the exterior spiral sulcus (sulcus spiralis externus), above which the thick, extremely vascular periosteum tasks as a spiral prominence. Above the prominence is a specialised, thick epithelial layer, the stria vascularis. The facet dealing with the scala vestibuli bears flattened perilymphatic cells, with tight junctions between them, making a diffusion barrier. The endolymphatic side is lined by squamous epithelial cells with many microvilli; these are additionally joined by tight junctions and are involved in ion transport. The organ of Corti, the sensory epithelium of the cochlea, sits on the basilar membrane. The apices of the sensory hair cells and the supporting cells it contains are joined by tight junctions to form the reticular lamina. The diffusion limitations that line the cochlear duct ensure that the apices of the sensory hair cells are bathed in endolymph, whereas their lateral and basal areas are bathed in perilymph. It is believed that calcium carbonate crystals from the otoliths become free of the otolithic membrane and, in certain positions, drop into the ampulla of the posterior semicircular canal, presumably turning into adherent to the cupula and rendering it gravity-sensitive. In sure positions, the alignment of the axis of the posterior semicircular canal with gravity results in the displacement of the cupula and the activation of the vestibuloocular reflex, resulting in compensatory nystagmoid eye actions in response to apparent head actions. Cure rates in excess of 80% have been recorded and the procedures have largely outdated surgical procedures designed to denervate the ampulla of the posterior semicircular canal (singular neurectomy) or obliterate the canal completely. Endolymphatic duct and sac the endolymphatic duct runs within the osseous vestibular aqueduct and becomes dilated distally to kind the endolymphatic sac. A, A horizontal part through the left temporal bone exhibiting the place of the cochlea with respect to the tympanic cavity. C, the structure of the cochlear organ of Corti and stria vascularis, showing the arrangement of the various types of cell and their general innervation. The group of the inner and outer hair cells and their synaptic connections are also depicted. It has a particular stratified epithelium containing a dense intraepithelial capillary plexus and three cell sorts: superficial marginal, dark or chromophil cells; intermediate mild, or chromophobe cells; and basal cells. The intermediate and basal cells lie deeper throughout the stria and ship cytoplasmic processes towards the surface, between the deeper parts of the marginal cells. The long descending cytoplasmic processes of the marginal dark cells and the ascending processes of the intermediate and basal cells envelop the intraepithelial capillaries. The stria vascularis is involved in ion transport and helps to produce the bizarre ionic composition of endolymph. It is the source of the massive constructive endocochlear electrical potential, upkeep of which is immediately dependent on enough oxygenation of the epithelial cells, offered by the intraepithelial capillary plexus. It consists of thick collagenous fibres interspersed with fibrocytic cells of several differing types, and root cells that ship large processes into the ligament from the area of the basilar crest. It ends externally within the internal spiral sulcus, which in part is formed like a C. Its upper part, the overhanging limbic edge, is the vestibular labium, and the decrease tapering half is the tympanic labium, which is perforated by small holes (the habenula perforata) for branches of the cochlear nerve. The upper surface of the vestibular labium is crossed at right angles by furrows, separated by numerous elevations � the auditory enamel (dentes acustici). During improvement, the interdental cells secrete some of the material that forms the tectorial membrane. Their bases rest on the basilar membrane near the tympanic lip of the internal spiral sulcus, and their bodies kind an angle of approximately 60� with the basilar membrane. Their heads resemble the proximal end of the ulna, with deep concavities for the heads of the outer pillar cells, which they overhang to kind the highest of the tunnel of Corti. They are longer and more oblique than the inside pillar cells, and type an angle of roughly 40� with the basilar membrane. The distances between the bases of the inside and outer pillar cells improve from the cochlear base to its apex, whereas the angles they make with the basilar membrane diminish. Cochlear hair cells are the sensory transducers of the cochlea; collectively, they detect the amplitude and frequency of the sound waves that enter the cochlea. The thin zona arcuata stretches from the spiral limbus to the bases of the outer pillar cells and supports the organ of Corti. It consists of compact bundles of small (8�10 nm diameter) collagenous filaments, primarily radial in orientation. The outer, thicker zona pectinata begins beneath the bases of the outer pillar cells and is hooked up to the crista basilaris. The basilar membrane is trilaminar in the zona pectinata, but the upper and decrease layers fuse at its attachment to the crista basilaris. The lower or tympanic surface of the basilar membrane is covered by a layer of vascular connective tissue and elongated perilymphatic cells. One vessel, the spiral vessel (vas spirale), is bigger; it lies instantly below the tunnel of Corti. The extra central of those structures are two rows of cells: the inner (inner) and external (outer) pillar cells. The bases of the pillar cells are expanded, and rest contiguously on the basilar membrane, but their rod-like cell bodies are widely separated. The apical ends of the hair cells and apical processes of the supporting cells kind an everyday mosaic called the reticular lamina, which is roofed by the tectorial membrane, a gel-like construction projecting from the spiral limbus. The reticular lamina is impervious to ions and thus maintains the electrochemical gradient between the fluids surrounding the apices and the basolateral membranes of the sensory hair cells. A slim gap separates the tectorial membrane from the reticular lamina except where the apical stereocilia of the outer hair cells project to make contact with it. In addition to the tunnel of Corti, different intercommunicating areas, the areas of Nuel, surround the outer hair cells. This entire intercommunicating advanced of areas of Nuel and tunnel of Corti is filled with perilymph, which diffuses via the matrix of the basilar membrane. Electron microscopy exhibits many microtubules, 30 nm in diameter, arranged in linked parallel bundles of 2000 or extra in the scapus, originating within the crus and diverging above the scapus to terminate in the head region. Three rows of V-shaped stereociliary bundles can be seen protruding from the apices of the outer hair cells. They are separated from the single row of inner hair cells (which have comparatively linear stereociliary bundles) by the apices of the inner pillar cells. B, the stereociliary bundle of one outer hair cell, exhibiting three rows of stereocilia increasing in height; deflection of the stereocilia in the course of the tallest row results in depolarization of the hair cell. The inset shows a tip link connecting a short stereocilium tip to the facet of the tall stereocilium behind. These two groups have distinctive roles in sound reception; the differences of their detailed structure mirror this useful divergence. The two sets of hair cells lean in path of one another apically at about the identical angles because the neighbouring inside and outer pillar cells. The geometric association of those cells is very exact, and this sample is carefully related to the sensory efficiency of the cochlea. The inner hair cells are surrounded by inner border cells and by inside phalangeal cells, which are attached externally to the heads of the internal pillar cells. The breadth of the apex exceeds that of the inside pillar cells so that every internal hair cell is related to more than one inner pillar cell. The apex bears 50�60 stereocilia, arranged in several ranks of progressively ascending height, the tallest on the strial aspect. The suggestions of the shorter rows are linked diagonally to the edges of the adjoining taller stereocilia by skinny filaments known as tip links; every stereocilium can also be linked to all its neighbours by a big selection of lateral links. The top of a stereociliary row varies along the length of the cochlea, being tallest at the apex and shortest at its base.
30 mg adalat mastercardWhen the arm is abducted blood pressure chart good and bad 30 mg adalat with amex, the head of the humerus may be palpated on deep stress within the apex of the axilla 01 heart attackm4a demi order adalat 30 mg on line. Distally hypertension remedies 20 mg adalat with amex, the medial humeral epicondyle is each visible and palpable arteria carotida externa 30 mg adalat discount with amex, particularly when the elbow is flexed, and could be traced proximally to the medial supracondylar ridge. The lateral epicondyle is much less prominent, however its posterior surface is palpable and its lateral margin may be traced proximally on deep palpation to the lateral supra condylar ridge. Inspection of the posterior surface of an prolonged elbow reveals a melancholy lateral to the midline, bounded laterally by the fleshy elevation shaped by the superficial forearm extensor muscular tissues, and medially by the lateral side of the olecranon. The floor of this depres sion accommodates the posterior floor of the lateral epicondyle superiorly, and the pinnacle of the radius covered by the anular ligament inferiorly. Rotations of the radial head are palpable throughout forearm pronation and supination. The humeroradial part of the elbow joint types a palpable transverse melancholy between the lateral epicondyle and the radial head. The posterior floor of the olecranon is subcutaneous and tapers because it passes inferiorly. When the elbow is flexed, the apex of the olecranon descends and the three bony factors then kind a triangle. The elbow joint is located 2 cm beneath a line joining the 2 humeral epicondyles. When the elbow is fully extended with the forearm and hand in supination, the carrying angle is often 165� in females and 175� in males. The angle is obscured in full forearm pronation and disap pears on full elbow flexion, when the shafts of the ulna and humerus come to lie in the same aircraft. The elbow joint can be accessed with a needle from a posterior perspective via the anconeus triangle; the borders of the triangle join the olecranon, radial head and lateral epicondyle. In distinction, the radial shaft is roofed by muscular tissues and can solely be felt indistinctly. The ulnar styloid process initiatives distally from the posteromedial facet of the ulnar head. The expanded distal end of the radius types a slight floor elevation on the lateral aspect of the wrist and could be traced downwards to the radial styloid process. The posterior facet of the decrease finish of the radius is partly obscured by the extensor tendons but may be palpated without problem. The tendon of extensor pollicis longus in extensor compartment three sits medial to the tubercle, and the tendons of extensor carpi radialis longus and brevis sit lateral to the tubercle in compart ment 2. The wrist joint is recognized between the distal ends of the radius and ulna and the proximal carpus on flexion and extension of the wrist. The line of the wrist joint corresponds to a line, convex superiorly, becoming a member of the radial and ulnar styloid processes. The radial styloid course of normally sits 1 cm distal to the ulnar styloid process. The pisiform is both visible and palpable on the palmar side of the medial wrist on the base of the hypothenar eminence. The tubercle of the scaphoid is situated at the base of the thenar emi nence, according to the tendon of flexor carpi radialis, and in plenty of individuals types a small visible elevation. Immediately distal to it, however lined by the muscular tissues of the thenar eminence, the tubercle of the trapezium could be identified on deep palpation. The heads of the metacarpal bones type the prominences of the knuckles, and are most obvious during digit flexion. Palpation distal to the meta carpal head reveals the flared base of the corresponding proximal phalanx. The interphalangeal joints are palpable on the dorsal facet of a flexed digit simply distal to the prominences fashioned by the heads of the proximal and middle phalanges. Key: 1, sternoclavicular joint; 2, clavicle; three, infraclavicular fossa/deltopectoral triangle, and deltopectoral groove operating inferolaterally; four, acromion; 5, deltoid; 6, pectoralis major; 7, lateral head of triceps; eight, biceps brachii; 9, median nerve and brachial artery running anterior to triceps medial head; 10, epicondylar line and borders of cubital fossa (blue); 11, brachioradialis; 12, pronator teres; 13, biceps tendon (black) and aponeurosis (grey) passing inferomedially; 14, extensor muscle mass; 15, cephalic vein. Key: 1, radial nerve; 2, brachial artery; 3, median nerve; 4, ulnar nerve (dashed part of line exhibits nerve passing posterior to medial epicondyle); 5, zone of radial nerve bifurcation (white): 1. The distal border is concave inferiorly and is marked by a curved line that joins the tubercle of the trapezium to the hook of the hamate. Its proximal border is marked by a curved line, concave superiorly, that joins the tubercle of the scaphoid to the pisi type. The dominant, most distal, wrist crease normally sits distal to the lunate and overlies pisiform and the proximal edge of the flexor reti naculum. The deltoid tendon is palpable roughly halfway down the lateral facet of the humerus. The posterior border runs superomedially from the posterior facet of the deltoid tendon and reaches the crest of the scapular spine close to its medial end. The normal rounded contour of the shoulder is produced by deltoid overlaying the lateral aspect of the greater tubercle of the humerus. Shoulder dislocation ends in the loss of the traditional rounded contour of the shoulder as a end result of the greater tubercle is displaced medially, and deltoid consequently descends verti cally to its humeral attachment. It is visible and palpable when an abducted shoulder is adducted against resistance. The clavicular head of pectoralis main could be felt and seen to contract when flexing the shoulder to a proper angle towards resistance; the sternocostal head becomes visible when extending a flexed shoulder against resistance. The posterior axillary fold, produced by latissimus dorsi and the underlying teres major, reaches a decrease stage on the humerus than the anterior axillary fold. When the abducted shoulder is adducted in opposition to resistance, the posterior axillary fold is accentuated and the lateral border of latissimus dorsi could be traced inferomedially to its attachment to the iliac crest. When the higher limb is raised above the pinnacle, the decrease 5 - 6 serrations of serratus anterior are seen on the lateral aspect of the thorax; they cross downwards and forwards to interdigitate with the serrations of exterior oblique. Flexion of the elbow against resistance aids identification of the muscle and of the bicipital tendon, which can be held between finger and thumb and traced down into the cubital fossa. With the elbow held in this place, the sharp upper margin of the bicipital aponeurosis could be traced passing inferomedially over the elevation produced by the superficial group of forearm flexor muscular tissues. Coracobrachialis emerges from the lateral axillary wall and forms a rounded ridge on the higher a part of the medial aspect of biceps. On the medial aspect, the fleshy mass produced by the lengthy head of triceps passes superiorly and disappears deep to deltoid. Brachioradialis is probably the most superficial muscle on the lateral side of the forearm. When the elbow is flexed in opposition to resistance whilst in a mid pronationsupination place, brachioradialis stands out as a promi nent ridge extending upwards beyond the extent of the elbow joint to the lower lateral aspect of the arm. The medial (ulnar) border of brachio radialis marks the boundary between the anterior and posterior forearm compartments. Pronator teres passes inferolaterally from the medial epicondyle to some extent approximately halfway down the radial shaft; its rounded stomach is visible throughout resisted forearm pronation. The fleshy mass of the superficial forearm flexors is visible and pal pable in the higher medial forearm, and that of the extensor muscle mass is seen in the higher lateral forearm. Key: 1, trapezius; 2, supraspinatus; three, spine of scapula; 4, acromion; 5, infraspinatus; 6, zone of axillary nerve passing round proximal humerus (white): approximately 6. A, Key: 1, radial artery; 2, flexor carpi radialis tendon; 3, median nerve; 4, ulnar nerve; 5, palmaris longus tendon; 6, flexor carpi ulnaris tendon; 7, proximal transverse wrist crease: marks the line of the wrist joint; 8, distal transverse wrist crease: marks the proximal boundary of the carpal tunnel; 9, scaphoid tubercle; 10, pisiform (black oval): aligns with distal wrist crease; eleven, trapezium tubercle; 12, hook of hamate and superficial department of ulnar nerve passing anteriorly; 13, thenar eminence; 14, hypothenar eminence; 15, aircraft of deep palmar arterial arch; 16, airplane of superficial palmar arterial arch; 17, positions of palmar digital neurovascular bundles; shaded rectangle signifies position of flexor retinaculum. Inflammation of the frequent flexor or extensor tendons could be indicated by tenderness to palpation over the respective muscle mass or humeral epicondyle. Palpating lateral to flexor carpi radialis, 3�4 cm proximal to the wrist crease, reveals the muscle stomach of flexor pollicis longus (flexing and extending the thumb will verify that the examining finger is accurately placed). The area on the ulnar facet of flexor carpi radialis tendon is full of functionally important buildings. The median nerve is both coated by, or situated just lateral (radial) to , the tendon of pal maris longus. Near to the wrist, the median nerve lies very near the skin and may, there fore, be injured by relatively superficial lacerations. When palmaris longus is absent, only a skinny overlaying of subcutaneous fat and deep fascia separate pores and skin and nerve. The 4 tendons of flexor digitorum superficialis lie deep to the median nerve; the tendons to the middle and ring fingers lie anterior to these for the index and little fingers as they pass deep to the flexor retinaculum, and could be felt and, normally, seen to move throughout finger flexion/extension. The snuffbox is bounded on its anterolateral (radial) side by the tendons of abductor pollicis longus (laterally) and extensor pollicis brevis (immediately medial), and on its posteromedial/ulnar side by the tendon of extensor pollicis longus.
Buy adalat 20 mg with mastercardAlthough this can be tougher in pigmented pores and skin heart arrhythmia xanax adalat 20 mg cheap otc, such adjustments are detectable hypertension range cheap 30 mg adalat amex. Paralysis entails biceps brachii blood pressure medication overdose treatment generic 20 mg adalat, brachialis blood pressure medication insomnia discount adalat 20 mg on-line, flexor carpi radialis and pronator teres. Paralysis is exten sive, and contains the long flexor muscles to the digits, the small muscular tissues of the hand, and the sleek muscle associated with the vessels and sweat glands supplying the ulnar three fingers. Anterior interosseous palsy is distinguished from excessive median harm by the absence of any loss of pores and skin sensation. There is a danger of underneath estimating the severity of a nerve lesion in circumstances of closed injury and after intraoperative occasions. Different populations of nerve fibres inside a primary nerve that has been violently stretched but not ruptured sustain lesions of all grades of severity. Testing of sensibility is often troublesome quickly after wounding, or when nerve damage is related to fracture of a long bone. The actions of some muscular tissues can be simulated by the actions of others, in order that the actual fact of paralysis can be missed in the early levels after nerve harm. Thus, when the median nerve has been reduce, opposition of the thumb could be mimicked by the action of extensor pollicis brevis (ulnar nerve) and abductor pollicis longus (radial nerve). Similarly, abductor pollicis longus can imitate the motion of the abductor pollicis brevis. One virtually infallible sign is all the time current in the first 48 hours after deep harm of a nerve with a cutane ous sensory part: as a outcome of small, in addition to large, fibres are affected, the skin in the distribution of the broken nerve is warm and dry. The injured hand or foot is placed, for a few minutes, in warm water; the skin of the denervated digits fails to wrinkle. In ischaemia, the massive fibres conveying discrimi native sensibility and vibration sense are first affected. Severance of a nerve with a cutaneous sensory component will lead to welldefined lack of sensi bility and to complete motor, sudomotor and vasomotor paralysis within the distribution of the nerve. Simple conduction block is likely to produce a patchy loss of sensibility and a patchy motor loss. The affected person is asked to say when the advancing finger elicits a wave or a surge of pins and needles or irregular sensations, which may be painful, into the distribution of the nerve, which must be clearly indicated by the examination iner. The level of the signal should be measured from a hard and fast bony point and the gap recorded. Preservation of the hypothenar muscle tissue with paralysis of the other hand muscle tissue internal vated by the ulnar nerve places a lesion in the proximal part of the palm of the hand. It signifies not only where the nerve has been injured but also the fact that no much less than some axons have been ruptured. It is tougher to elicit the sign over deepseated nerves such as the axillary, eighth cervical or first thoracic nerves. Although nerve conduction is lost before muscle contractility, ischaemia is extra prone to produce infarction of muscle than necrosis of nerve. Decompression of a nerve embedded inside muscle that has become fibrosed by ischaemia often leads to reduction of ache and con siderable enchancment in sensation and sympathetic perform, even when delayed for some months. Anoxia happens both due to cessation of flow via a major axial artery or as a outcome of growing stress within an osseofascial compartment brought on by bleeding, infusion of fluid or sepsis. It destroys the integrity of the cell membrane and capillary endothelium, which signifies that the homeostatic steadiness between the intravascular, extracel lular and intracellular areas is misplaced. The elevated permeability of the vascular endothelium leads to an increase in intracompartmental strain by exudation, which collapses the lowpressure lymphatic and venous systems. The final occasion is the closure or obstruction of perfusing arterioles to muscles and the extrin sic provide to nerves, when tissue or extravascular pressure exceeds the cortical closing strain of these vessels. Increasing intracompartmental pressure occurs when the col lateral circulation is inadequate after occlusion of the main artery or after restoration of move by way of that vessel, except the compartments have been decompressed adequately by fasciotomy. The vascular anas tomoses about the joints of the higher limb provide a richer collateral circulation than these discovered in the lower limb. In contrast, the incidence of amputation after ligation was about onequarter for the subclavian artery, onethird for the axillary artery and more than onehalf when the brachial artery was ligated proximal to the profunda brachii artery. These figures are cer tainly decrease in the much less contaminated accidents of civilian life, but some degree of postischaemic fibrosis is sort of inevitable after failure to repair these vessels. The rules of arterial repair embody urgent restoration of flow by restore of the artery and restoration of tissue per fusion by decompression. Temporary intraluminal shunts are invalua ble, as they buy time and permit enough stabilization of the skeleton. Application of these ideas in present conflicts ensures a remarkably high fee of limb survival and a remarkably low incidence of publish ischaemic fibrosis. Flow by way of the brachial artery in adults and in children has been measured by highresolution ultrasonography. The mean diameter of the brachial artery in youngsters aged between four and 5 years is 2. This is the bodily legislation describing the amount of circulate of an incompressible uniform viscous liquid, where R is the inner radius of the tube, P the stress distinction between the two ends, the dynamic fluid viscosity and L the whole length of the tube. However, direct stimulation of the muscle provokes a twitch that could be elicited for up to a quantity of hours. Sleeves of fascia encompass primary nerves and primary vessels in some areas, an association that predisposes nerves to injury from ischae mia or compression, or each. The ventral (anterior) main rami of C7, C8 and T1 are enclosed in fairly a inflexible area after they enter the posterior triangle of the neck. This is bounded, posteriorly, by the dorsal part of the primary rib, the transverse processes of the cervical vertebrae and by the fascia of levator scapulae. The nerves are embraced by scalenus anterior and scalenus medius, each of that are invested in an unyield ing fascia. This is one envelope of the prevertebral fascia that additionally serves to bind the phrenic nerve all the means down to the anterior face of scalenus anterior. The prevertebral fascia is especially well developed in front of the vertebral column and also on the base of the posterior triangle, where it envelops C7, C8 and T1, the phrenic nerve, the cervical sympathetic chain, and the subclavian and vertebral arteries. Infusion of relatively massive volumes of fluid, from 10 to 20 ml, deep to the prevertebral fascia for the purpose of inducing regional block could trigger tamponade of the radicular vessels that enter the spinal canal and contribute to the anterior spinal artery. Wilbourn (2005) has described the medial bra chial fascial compartment, which extends from the axilla to the elbow and is bounded by the robust medial intramuscular septum and the axillary sheath. Bleeding into this compartment is responsible for the majority of infraclavicular plexopathies that follow regional block, and for many of the neurological lesions that outcome from closed or even open injuries on this region. The anterior interosseous nerve and its accompanying artery may be damaged by compression because of swelling within the deepest part of the flexor compartment of the forearm. The ulnar nerve, accompanied by the ulnar artery, lies in a discrete fascial compartment within the distal twothirds of the forearm. Bleeding into the axillary fascia (the medial antebrachial compart ment) causes a characteristic, progressive lesion. There is, nearly all the time, ache accompanied by dysaesthesiae; loss of sensation quickly follows after which, over the subsequent 2�3 hours, paralysis ensues. In one collection of 16 patients (Stenning et al 2005), there was, in all circumstances, an injury to the axillary artery or certainly one of its offsets, brought on by dislocation of the shoulder or fracture of the proximal humerus. The diagnosis of constant bleeding into the axillary sheath was made by the delayed onset of nerve palsy or the deepening of the lesion while beneath obser vation. A beneficial consequence was seen in 87 nerve palsies, where pressing restore of the artery and decompression of the axillary sheath had been per fashioned. This calibre provides move of about 20 ml per minute, assuming that the pressure gradient is identical as that in the brachial artery itself. These information must be borne in thoughts by any clinician inclined to the view that cessation of move by way of the brachial artery is a matter of little consequence. The collateral channels take hours or days to develop and could also be compromised by the original injury or throughout operation. The radial and ulnar nerves are often entrapped or compressed in fracture dislocations on the elbow, blocking move through the ulnar and radial collateral systems that accompany these nerves. The cardinal symptom of ischaemic anoxia is extreme ache and the cardinal sign is lack of nerve conduction.
20 mg adalat cheap mastercardA native speaker of any language can quickly acknowledge the origins of anybody making an attempt to use their language as a second language hypertension management guidelines 30 mg adalat best. Similarly arteria umbilical percentil 90 adalat 20 mg discount line, the way of articulation can vary from a complete closure to a slight narrowing hypertension lifestyle modification discount adalat 20 mg on-line. Approximants involve a level of closure inadequate to produce turbulence however with closure greater than that for a vowel blood pressure medication bananas buy generic adalat 30 mg online. Nasals contain a stoppage in the oral cavity with the taste bud lowered to allow airflow through the nose, and, unlike stops, they can be sustained. The finest approach to illustrate these classificatory techniques in operation is by contrasting the manufacturing of various consonant pairs during which just one or two parameters have been changed. The distinction between the /b/ and the /p/ is within the differing means during which the airstreams are produced. The /b/ is produced with an egressive pulmonary airflow, while the /p/ is produced with the glottis closed � therefore is unvoiced � and the glottis is then raised using the larynx as a piston to compress the air within the supralaryngeal vocal tract previous to the cease being launched. The /m/ differs from the other two stops in being a nasal by which the soft palate is lowered to permit air to escape by way of the nasal cavity; in distinction to the other two stops, it could be sustained as in a sound of approval. Bilabial stops can be contrasted with the labiodental fricatives /f/ of feet and the /v/ of veal, each of that are produced by retracting the lower lip beneath the upper tooth. Neither involves a complete closure but each produce a major constriction of the vocal tract with audible turbulence: the /f/ is unvoiced, whereas the /v/ is voiced. The sh sound (//) in ship can be a fricative involving a grooving of the tongue and is related to important audible turbulence; it may be contrasted with the lateral approximant /l/ in regulation, in which the edges of the tongue are lowered. The sh sound in ship could be in comparison with the /k/ in eager, where the place of the tongue is completely different: in /k/ the tongue blade contacts the soft palate, whereas in sh the tongue tip or the blade contact the postalveolar area. The most dramatic instance of the distinction between voiced and unvoiced sounds may be appreciated if the /s/ sound in sip is in contrast with the /z/ in zip. The position of the tongue and different articulators is strictly the same for both /s/ and /z/; the distinction between them is the presence or absence of phonation. A comprehensive summary of the natural problems of voice because of laryngeal structural modifications and neurological disease, in addition to psychogenic voice disorders. A discussion of the routes of lymphatic drainage from the larynx and related structures. Atkinson M, McHanwell S 2002 Basic Medical Science for Speech and Language Therapy Students. A description of all elements of laryngeal anatomy, together with a really useful bibliography. A e-book dealing with the evaluation, analysis and administration of sensory and motor problems of the larynx. Clark J, Yallop C, Fletcher J 2007 An Introduction to Phonetics and Phonology, 3rd ed. Fayoux P, Devisme L, Merrot O et al 2004 Histologic structure and development of the laryngeal macula flava. Hatley W, Samuel S, Evison G 1965 the pattern of ossification within the laryngeal cartilages: a radiological examine. An older textbook that contains lots of helpful data not in any other case readily available. Kochilas X, Bibas A, Xenellis J et al 2008 Surgical anatomy of the external branch of the superior laryngeal nerve and its medical significance in head and neck surgery. Liu M, Chen S, Liang L et al 2013 Microcomputed tomography visualisation of the cricoarytenoid joint cavity in cadavers. Maranillo E, Leon X, Orus C et al 2005 Variability in nerve patterns of the adductor muscle group provided by the recurrent laryngeal nerve. Maranillo E, Vazquez T, Ibanez M et al 2008 Anatomic examine of human laryngeal ganglia: number and distribution. Monfared A, Gorti G, Kim D 2002 Microsurgical anatomy of the laryngeal nerves as related to thyroid surgery. Mu L, Sanders I 2009 the human cricothyroid muscle: three muscle bellies and their innervation patterns. Sato I, Shimada K 1995 Arborization of the inferior laryngeal nerve and internal nerve on the posterior surface of the larynx. Sato K, Umeno H, Nakashima T 2010a Functional histology of the macula flava within the human vocal fold � half 1: its role in the grownup vocal fold. Sato K, Umeno H, Nakashima T 2010b Functional histology of the macula flava in the human vocal fold � half 2: its function in the progress and development of the vocal fold. Storck C, Gehrer R, Fischer C et al 2011 the position of the cricothyroid joint anatomy in cricothyroid approximation surgical procedure. Strauss S 2000 Sonographic appearance of cricoid cartilage calcification in healthy children. Vazquez T, Cobiella R, Maranillo E et al 2009 Anatomical variations of the superior thyroid and superior laryngeal arteries. This chapter will provide an outline of head and neck growth based totally on knowledge from research on human embryos. Evolution of the vertebrate head was made attainable by the origin of a novel cell inhabitants, the neural crest. Neural crest cells have the potential to kind connective and skeletal tissues within the head, and so they make main contributions to the cranium. In mammalian embryos, cranial neural crest cells emigrate from the edges of the still-open cranial neural folds, unlike trunk neural crest cells and the cranial crest of other vertebrates, which begin migration solely after neural tube closure. In the mouse, a lineage marker has enabled neural crest cells to be traced from the stage at which they go away the neural epithelium by way of to their last locations in mature tissues. Those neural crest cells with a neuronal destiny contribute to A Oropharyngeal membrane Amnion Pharyngeal part of foregut Preotic sulcus Otic sulcus Heart Heart Notochord Yolk sac wall Closed neural tube Connecting stalk 36 the trigeminal ganglion. The second (hyoid) population provides rise to the otic ganglion after which migrates from prorhombomere B (which forms rhombomeres 3 and 4), into the second pharyngeal arch. The third (vagal) population has a more extensive origin, from the neural folds caudal to the otocyst, i. These cells will contribute to the ganglia of the glossopharyngeal and vagal nerves, with the non-neuronal vagal crest cells migrating into pharyngeal arches 3, four and 6, some of them persevering with into the center to contribute to the division of the cardiac outflow tract (Jiang et al 2000). The neural crest additionally offers rise to the parasympathetic ganglia and parasympathetic postganglionic nerves in the head and neck. For a full account of the neuronal contribution of neural crest cells, see Chapter 17. Caudal to the segmented region of the cranial neural tube, neural crest cells from the occipital area (prorhombomere D/rhombomere 8) migrate with occipital myoblasts to kind the hypoglossal wire, ultimately differentiating to kind the connective tissue (neural crest) and musculature (myoblasts) of the tongue. Ectodermal placodes seem as patches of columnar or pseudostratified epithelium inside the otherwise squamous epithelium of the surface ectoderm. Three pairs of placodes contribute to sense organs, forming the olfactory epithelium, the lens and the otocyst, present process morphogenesis to type a pit and then (for the lens and otic pits) a closed cyst (vesicle). A, A sagittal part of a stage 10 embryo, in which neural tube closure has begun in the future occipito-cervical area. This early division is of major practical and organizational significance, because it separates the areas of origin of the skeletogenic neural crest populations that make a significant contribution to the skull from those who type skeletal structures in the neck (hyoid bone and larynx). Genetic experiments in the mouse and other vertebrates have shown that skeletal patterning of the first pharyngeal arch is dependent upon the absence of Hox gene expression in the neural crest cells migrating into it; skeletal patterning of the second arch depends on the expression of Hoxa2. Investigation of Hox gene expression in arches 3�6 has not revealed clear skeletal patterning features. A�B, Scanning electron micrographs (A, dorsal view; B, median section) of embryos close to the beginning (4 somite pairs) and finish (18 somite pairs, inside view) of the period of neural crest cell migration. At the 4-somite stage, the neural folds are convex and the hindbrain is divided into prorhombomeres A, B and C by the preotic (arrow) and otic (arrowhead) sulci; on the 18-somite stage, the neural tube is closed and the hindbrain is divided into seven rhombomeres (numbered) and the unsegmented occipital area (oc). C�D, Lateral views of embryos at the 5- and 23-somite stage, respectively, carrying a everlasting marker for neural crest cells and the neural epithelium from which the trigeminal crest cells originate (blue stain). Trigeminal neural crest cells (nc) migrate as a veil-like mass beneath the floor ectoderm, originating as a steady group from prorhombomere A, the midbrain and the caudal diencephalic region (d) of the forebrain, into the frontonasal area (fn) and the first arch (white lines indicate the level of the migrating edge). After migration, frontonasal neural crest cells (fn) cover the telencephalon and rostral diencephalon, surrounding the eye (e); maxillary (mx) and mandibular (md) neural crest populates the primary pharyngeal arch; the trigeminal ganglion primordium (V) can also be current. The epithelial to mesenchymal transformation of some cells from ectodermal placodes contributes a third element to the cranial mesenchyme.
Discount adalat 20 mg with amexThe cricoid cartilage arises from two cartilaginous centres blood pressure medication without hair loss adalat 20 mg buy online, which quickly unite ventrally arteria epigastrica cranialis superficialis adalat 20 mg fast delivery, gradually lengthen arteria y vena femoral discount 20 mg adalat, and in the end fuse on the dorsal floor of the tube because the cricoid lamina hypertension jnc 8 guidelines pdf adalat 20 mg order on line. Paired arytenoid swellings appear within the ventral tissue of the sixth arches from stage 14, one on each side of the cranial finish of the laryngotracheal groove. As they enlarge, they approximate to one another and to the caudal part of the hypobranchial eminence, the place the epiglottis develops. The opening into the larynx, at first a simple slit, is converted into a T-shaped cleft by the enlargement of the arytenoid swellings. The vertical limb of the T lies between the 2 swellings, and its horizontal limb lies between them and the epiglottis. Laryngeal and tracheobronchial veins also drain to the precardinal advanced, whilst the capillary plexuses, developed within the (splanchnopleuric) walls of the nice terminal respiratory passages and alveoli, converge on pulmonary veins of accelerating calibre, lastly making secondary connections with the left atrium of the heart, and may be grouped with the vitelline methods. The notochordal sheath is wealthy in sulphated glycosaminoglycans, which play a task in inducing condensation and chondrification of the occipital sclerotome-derived mesenchyme round it. Laterally, the exoccipital parts (derived from sclerotomes 3 and 4) chondrify quickly afterwards; they lengthen across the hindbrain to kind the occipital arch, which is developmentally equal to the neural arch components of vertebrae. The supraoccipital part of the occipital cartilage extends dorsally from the exoccipital cartilage to complete the foramen magnum. After formation of the exoccipital cartilages, differentiation also extends further rostrally in the medial part of the skull base, with formation of the hypophysial polar cartilages on both side of the hypophysial stalk; they unite in the median airplane to form the primordium of the postsphenoid, cradling the hypophysis and retaining a perforation for the hypophysial stalk until the third month. This part of the basisphenoid cartilage will form the sella turcica with its hypophysial fossa. This is the final a half of the medial part of the skull base to differentiate as cartilage, bridging the hole between the postsphenoid and the cartilaginous nasal capsule. At stage 17, mesenchyme begins to condense and later to chondrify around the nasal pits, forming the outer part of the nasal capsule and the nasal septum; the roof of every nasal capsule is completed slightly later, when cartilage differentiates around the olfactory nerve bundles to form the cribriform plates of the ethmoid bone. The whole nasal capsule is nicely developed by the top of the third month, and consists of a common median septal half, typically initially termed the interorbitonasal septum or mesethmoid, and the outer ectethmoid. The conchae ossify through the fifth month; the superior and center conchae kind a half of the ethmoid bone, and the inferior pair turn into separate elements. Part of the capsule stays cartilaginous because the septal and alar cartilages of the nose, and half is replaced by the intramembranous vomer and nasal bones. The most rostral of them becomes steady with the presphenoid cartilage by differentiation of a cartilaginous bridge that forms the caudal boundary of the optic foramen, enclosing the optic nerve; this later ossifies to form the lesser wing of the sphenoid bone (orbitosphenoid). The greater wing of the sphenoid (alisphenoid) has each intramembranous and endochondral components; the endochondral half initially differentiates as a cartilage surrounding the mandibular department of the trigeminal nerve, forming the foramen ovale. This condensation extends medially to join the rostral fringe of the hypophysial (polar) cartilage on both sides. It additionally extends rostrally to surround the maxillary branch of the trigeminal nerve, forming the foramen rotundum. Lastly, it extends laterally to join the intramembranous part of the bone, which replaces the caudal a half of the orbital cartilage. The greater and lesser wings of the sphenoid are separated by the oculomotor, trochlear and abducens nerves and by the primary (ophthalmic) division of the trigeminal nerve. The otic capsule differentiates from a mesenchymal condensation around the otocyst, after its morphogenesis to type the cochlea and semicircular canals. Chondrogenesis across the level of exit of the vestibulocochlear nerve creates the inner acoustic meatus. Chondrogenesis of mesenchyme around the carotid arteries joins every hypophysial cartilage to the otic capsule, forming the carotid canals. A gap occupied by the jugular vein and the glossopharyngeal, vagus and accessory nerves stays between each otic capsule and the parachordal cartilage; this is the jugular foramen. The neurocranium is composed of the calvaria and basicranium; it surrounds and protects the mind and the particular sense organs of olfaction, imaginative and prescient, listening to and steadiness. The viscerocranium, which incorporates the squamous part of the temporal bone, varieties the skeleton of the face, palate and pharynx, and mediates the features of feeding, respiratory and facial expression; it additionally protects the tongue and forms the middle ear and the bony exterior acoustic meatus. The boundary between neural crest and cranial mesoderm lies between the frontal and parietal bones (coronal suture) of the calvaria; the cranium base is fashioned by neural crest rostral to the tip of the notochord, and is sclerotome-derived. Broadly talking, the bones of the skull base are shaped by endochondral ossification (chondrocranium), whereas these of the calvaria and face ossify immediately from mesenchymal condensations, i. Several bones are of compound construction with respect to their tissue origins and/or kind of ossification: the occipital, temporal and sphenoid bones, and the mandible. Development of the pharyngeal arch-related cartilages of the viscerocranium and ear ossicles has been described in the section on the pharynx. In all of the diagrams, the chondrocranium and cartilaginous levels of vertebrae are shown in blue, besides the place ossification is going on; right here, the colour is green. A, A sagittal part via the cranial finish of the creating axial skeleton in an early human embryo of roughly 10 mm (5 weeks), displaying the extent of the notochord. The remnant of the hypophysial stalk is indicated by a black dot within the hypophysial fossa. The process of endochondral ossification in the skull is essentially the identical as that of the long bones, besides that every ossification centre is equal to a major centre, and follows a particular programme of progress and patterning. Growth takes place inside the cartilage between adjoining ossification centres; these joints are termed synchondroses. The first ossification centres to seem are these of the lesser and greater wings of the sphenoid, at 8 and 9 weeks, respectively. A single basisphenoid ossification centre seems at eleven weeks; three presphenoid and four postsphenoid ossification centres appear at sixteen weeks. Bone replaces most of the cartilage till solely the main synchondroses stay; these allow the endochondral skull base and sensory capsules to proceed rising until they reach their final measurement at puberty or earlier. At delivery, unossified chondrocranium persists in the alae, lateral nasal cartilage and septum of the nose, the sphenoethmoidal junction, the sphenooccipital and sphenopetrous junctions, the apex of the petrous temporal bone (foramen lacerum), and between ossification centres of the sphenoid and occipital bones. In common, endochondral ossification centres type later than intramembranous ossification websites, which first appear in the course of the seventh and eighth weeks. In humans, as in all mammals, the most important part of the calvaria is shaped by paired frontal and parietal bones and the unpaired interparietal (membranous a part of the occipital bone). The squamous a part of the temporal bones and the alisphenoids contribute to the lateral partitions. Lineage data from mouse research point out that the frontal and squamous temporal bones are of neural crest origin and the parietals are of mesodermal origin; the interparietal is combined (Jiang et al 2002). The coronal suture thus forms on the neural crest�mesoderm interface, as does the sagittal suture, due to a small tongue of neural crest tissue lying between the 2 creating bones. These tissue interfaces are important for initiating the molecular signalling system that governs growth of the calvaria. In addition to the expansion-related growth that takes place in the sutures, appositional growth, by which bone is laid down on, and resorbed from, the bone surfaces, plays an essential position in remodelling the calvarial bones to maintain a degree of curvature that matches the curved floor of the rising brain. The frontal and parietal bones are initiated as basolateral mesenchymal primordial, which extend upwards between the dermal connective tissue and the mesenchymal dura mater. As the frontal and then the parietal primordia prolong upwards, the differentiating osteoblasts secrete osteoid, which then undergoes mineralization. Only the mineralized components of the bones are detected in alizarin-stained specimens and X-rays. Clear frontal bone primordia are detectable within the superciliary arch region of alizarinstained human embryos by the eighth week. As they become mineralized above this degree, the parietal bone primordia may additionally be seen. The two bones seem to be separated by a large hole on the coronal suture; in reality, this gap solely shows the separation of the mineralized parts of the bone � the unmineralized fringe of the parietal bone truly overlaps the caudal fringe of the frontal bone. During vaginal start, the overlap of the frontal and parietal bones allows them to slide over one another. During the neonatal interval, when the baby cries and intracranial pressure rises, the overlapping bones slide aside, growing the fronto-occipital diameter of the cranium. Growth at the coronal suture supplies the most important increase within the frontooccipital airplane of the calvaria. Premature synostosis of the coronal sutures restricts progress in this aircraft, inflicting brachycephaly; unilateral coronal synostosis results in plagiocephaly, in which one side of the cranium fails to grow within the fronto-occipital plane. Uni- and bilateral coronal synostosis comprises 20�25% of all forms of craniosynostosis. The metopic and sagittal sutures are fashioned when the upwardly extending frontal and parietal bones (respectively) reach the vertex of the cranium and abut within the median aircraft.
|
|