|
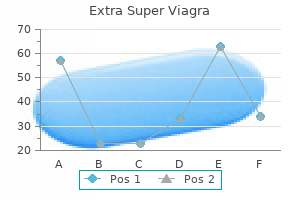
"Order extra super viagra american express, erectile dysfunction caused by radical prostatectomy". E. Candela, M.A., M.D., M.P.H. Co-Director, Weill Cornell Medical College
Management of anesthesia in sufferers with von Hippel� Lindau illness should think about the possible presence of a pheochromocytoma. Preoperative therapy with antihypertensive medication is indicated if a pheochromocytoma is identified. The chance of spinal cord hemangioblastomas may restrict the utilization of spinal anesthesia, though epidural anesthesia has been described for cesarean part. Exaggerated hypertension, especially during direct laryngoscopy or sudden adjustments within the depth of surgical stimulation, may require intervention with esmolol, labetalol, sodium nitroprusside, or a combination of those medication. The range of scientific features of neurofibromatosis emphasizes the protean nature of this disease (Table 10-8). Caf� au lait spots (abnormal cutaneous pigmentation) are current in virtually every affected individual. Caf� au lait spots are often present at start and continue to enhance in quantity and measurement through the first decade of life. These neurofibromas may be nodular and discrete or diffuse with intensive interdigitations into surrounding tissues. Although neurofibromas are histologically benign, functional compromise and cosmetic disfigurement could outcome from their presence. The airway may be compromised when neurofibromas develop in the laryngeal, cervical, or mediastinal regions. Intracranial tumors happen in 5% to 10% of patients with neurofibromatosis and account for a major portion of the morbidity and mortality of this illness. The bilateral presence of acoustic neuromas in patients with caf� au lait spots establishes the prognosis of neurofibromatosis. Congenital pseudoarthrosis-that is, a spontaneous fracture that progresses to nonunion-is commonly encountered in neurofibromatosis. The severity of pseudoarthrosis ranges from an asymptomatic radiographic presentation to a severe nonunion requiring limb amputation. Paravertebral neurofibromas are sometimes present, however their position, if any, within the improvement of kyphoscoliosis is unclear. Untreated, kyphoscoliosis typically progresses, resulting in cardiorespiratory and neurologic compromise. These embody pheochromocytoma, disturbances in sexual growth, medullary thyroid carcinoma, and hyperparathyroidism. Seizures might complicate neurofibromatosis and could additionally be idiopathic or mirror the presence of intracranial tumors. Treatment of neurofibromatosis consists of drug therapy as wanted to deal with symptoms, corresponding to antiepileptic medication, and appropriately timed surgery. Surgical elimination of cutaneous neurofibromas is reserved for these lesions that are significantly disfiguring or trigger practical issues. The attainable presence of a pheochromocytoma should be thought of through the preoperative analysis. Patients with neurofibromatosis and scoliosis are more doubtless to have cervical spine defects that could affect positioning for direct laryngoscopy and the next surgical process. These patients have been described as each sensitive and immune to succinylcholine and delicate to nondepolarizing muscle relaxants. Selection of regional anesthesia should think about the possible future improvement of neurofibromas involving the spinal wire. Epidural analgesia is an efficient methodology for producing analgesia during labor and delivery. Patients are sometimes confused and sometimes uncooperative, which makes monitored anesthesia care or regional anesthesia challenging. Shorter-acting sedative-hypnotic drugs, anesthetic agents, and narcotics are preferred since they permit a more rapid return to baseline mental status. One ought to be aware of potential drug interactions, especially prolongation of the impact of succinylcholine and relative resistance to nondepolarizing muscle relaxants ensuing from the use of cholinesterase inhibitors. Increasing age is the one most essential danger issue in the development of this illness. There is a characteristic lack of dopaminergic fibers normally current in the basal ganglia, and as a result, regional dopamine concentrations are depleted. Dopamine is presumed to inhibit the rate of firing of the neurons that control the extrapyramidal motor system. Depletion of dopamine ends in diminished inhibition of those neurons and unopposed stimulation by acetylcholine. The earliest manifestations may be loss of related arm swings when walking and absence of head rotation when turning the physique. There is facial immobility manifested by infrequent blinking and by a paucity of emotional expressions. Tremors are characterized as rhythmic, alternating flexion and extension of the thumbs and other digits (pill-rolling tremor). Tremors are more distinguished during relaxation and have a tendency to disappear throughout voluntary motion. Replacement remedy with the dopamine precursor levodopa combined with administration of a decarboxylase inhibitor, which prevents peripheral conversion of levodopa to dopamine and optimizes the quantity of levodopa available to enter the central nervous system, is the usual medical therapy. Levodopa is related to a variety of unwanted effects, together with dyskinesias and psychiatric disturbances. The elevated myocardial contractility and coronary heart rate seen in handled sufferers could reflect elevated levels of circulating dopamine transformed from levodopa. It is the most common explanation for dementia in patients older than 65 years of age and the fourth most common reason for diseaserelated dying in patients older than age 65. Diffuse amyloidrich senile plaques and neurofibrillary tangles are the hallmark pathologic findings. There are additionally changes in synapses and within the activity of several main neurotransmitters, especially involving acetylcholine and central nervous system nicotinic receptors. In each forms of the disease, sufferers typically develop progressive cognitive impairment that may consist of issues with reminiscence in addition to apraxia, aphasia, and agnosia. Pharmacologic options include cholinesterase inhibitors corresponding to tacrine, donepezil, rivastigmine, and galantamine. Drug remedy should be combined with nonpharmacologic remedy including caregiver education and family support. Stimulation of the various nuclei within the basal ganglia through an implanted deep mind stimulating device can relieve or help to control tremor. Pallidotomy is associated with significant improvement in levodopa-induced dyskinesias, though the development could additionally be short-lived. However, in certain circumstances, corresponding to in patients with developmental delay or these with extreme claustrophobia, the procedure is carried out underneath general anesthesia. The deep brain electrode is then superior via a burr gap, usually with microelectrode recordings taken, since particular nuclei differ in their spontaneous firing patterns. The target tissue is then stimulated by way of the electrode to determine if clinical symptoms abate. Following profitable brain lead placement, a generator pack is implanted under the clavicle or in the abdomen. Of observe, deep mind stimulation is presently beneath investigation for remedy of a wide selection of other issues, such as Hallervorden-Spatz disease, melancholy, and consuming issues. The elimination half-time of levodopa and the dopamine it produces is brief, so interruption of drug remedy for more than 6 to 12 hours can result in an abrupt loss of therapeutic effects. Abrupt drug withdrawal also can lead to skeletal muscle rigidity, which may intervene with ventilation. Therefore, levodopa remedy, together with the standard morning dose on the day of surgery, have to be continued throughout the perioperative interval. Oral levodopa can be administered roughly 20 minutes earlier than induction of anesthesia, and the dose may be repeated intraoperatively and postoperatively by way of an orogastric or nasogastric tube as wanted. The chance of hypotension and cardiac dysrhythmias must be considered, and butyrophenones. Acute dystonic reactions following administration of alfentanil would possibly point out an opioidinduced decrease in central dopaminergic transmission.
Diseases - Bethlem myopathy
- Multiple congenital anomalies mental retardation, growth failure and cleft lip palate
- Congenital kidney disorder
- Alternating hemiplegia of childhood
- Panophobia
- Chronic berylliosis
- Prieto Badia Mulas syndrome
- Craniosynostosis, sagittal, with Dandy-Walker malformation and hydrocephalus
Double Aortic Arch Double aortic arch results in a vascular ring that can produce pressure on the trachea and esophagus. Compression resulting from this pressure can be manifested as inspiratory stridor, problem mobilizing secretions, and dysphagia. Patients with this cardiac defect often favor to lie with the neck extended because flexion of the neck usually accentuates compression of the trachea. Surgical transection of the smaller aortic arch is the treatment of choice for symptomatic sufferers. During surgery, the tracheal tube must be placed beyond the realm of tracheal compression if this might be safely completed with out producing endobronchial intubation. It must be appreciated that esophageal stethoscopes or nasogastric tubes could cause occlusion of the trachea if the tracheal tube stays above the extent of vascular compression. In addition to hemodynamic elements, weaning from mechanical air flow should bear in mind the risk of tracheomalacia caused by extended compression of the trachea, which may jeopardize the patency of the trachea. Aberrant Left Pulmonary Artery Tracheal or bronchial obstruction can occur when the left pulmonary artery is absent and the arterial supply to the left lung is derived from a department of the best pulmonary artery passing between the trachea and esophagus. The sling may cause obstruction of the right major bronchus, the distal trachea, or rarely the left main bronchus. Clinical manifestations of an aberrant left pulmonary artery embrace stridor, wheezing, and sometimes arterial hypoxemia. Unlike with a real vascular ring, esophageal obstructions are uncommon, and the stridor produced by this defect is usually current throughout exhalation quite than inspiration. Chest radiographs may demonstrate an irregular separation between the esophagus and the trachea. Surgical division of the aberrant left pulmonary artery at its origin and redirection of its course anterior to the trachea, with anastomosis to the primary pulmonary artery, is the therapy of selection. During the primary months of life, surgical correction with deep hypothermia without cardiopulmonary bypass could also be considered. Absent Pulmonic Valve Absence of the pulmonic valve leads to dilation of the pulmonary artery, which may finish up in compression of the trachea and left primary bronchus. This lesion might occur as an isolated defect or at the aspect of tetralogy of Fallot. Symptoms include indicators of tracheal obstruction and sometimes the development of arterial hypoxemia and congestive heart failure. Any increase in pulmonary vascular resistance, as could happen with arterial hypoxemia or hypercarbia, accentuates airway obstruction. Tracheal intubation and maintenance of four to 6 mm Hg of steady constructive airway strain can be utilized to maintain the trachea distended, which reduces the magnitude of airway obstruction. Definitive remedy consists of inserting a tubular graft with an artificial pulmonic valve. In either case, grownup sufferers with congenital heart illness should be handled optimally by clinicians with expertise in the physiology of congenital heart disease and its manifestations within the mature particular person. Therefore, knowledge of and expertise with the physiology of adult congenital heart illness and its challenges is paramount for the anesthesiologist during the perioperative period. In the United States alone there are more grownup patients with congenital coronary heart disease than pediatric sufferers with these problems, and the number of surviving citizens is estimated to be between 1 million and a pair of. The prevalence of extreme congenital heart disease in grownup patients increased by 85% from 1985 to 2000, significantly outpacing that within the pediatric inhabitants. The majority of the mortality and morbidity in these patients can be attributed to chronic difficulties, namely, cardiovascular causes similar to continual coronary heart failure. In two large cohorts, hospitalization charges have been 50%, twice that of the overall population. Long-term cardiac complications include pulmonary hypertension, ventricular dysfunction, dysrhythmias and conduction defects, residual shunts, valvular lesions (regurgitation and stenosis), hypertension, and aneurysms. A vital variety of these patients require extra cardiac surgeries to address residual lesions, corresponding to atrioventricular valve regurgitation, pulmonary valve regurgitation, outflow tract obstruction, or arrhythmias. In nearly all instances, congenital heart illness in adults must be viewed as a systemic situation with associated multiorgan dysfunction. Perioperative threat is substantially increased in adults with congenital coronary heart illness, significantly those with poor functional status, pulmonary hypertension, congestive heart failure, and cyanosis. With every lesion, there are unique manifestations require a meticulous perioperative plan. Premedication is advantageous in these grownup congenital coronary heart illness sufferers with anxiousness because of a quantity of prior procedures or developmental delay (trisomy 21) however have to be undertaken cautiously, as a outcome of hypercapnia and hypoventilation can improve pulmonary vascular resistance and be deleterious to patients with pulmonary hypertension or systemic-to-pulmonary shunts. The most typical form of tachyarrhythmia noticed is intraatrial reentrant tachycardia originating from the best atrium, which could be immune to pharmacologic remedy and result in speedy hemodynamic deterioration. Pulmonary hypertension poses one other danger issue to adults with congenital heart disease. It may be as a outcome of pulmonary venous hypertension secondary to elevated ventricular enddiastolic stress, elevated pulmonary venous atrial pressure, or pulmonary vein stenosis. Although some patients might have decreased oxygen saturation resulting from residual shunt or poor lung perform, the primary reason for pulmonary hypertension in adults with congenital heart illness is the presence of persistent giant and nonrestrictive shunts. The increased blood circulate and near systemic pressure to the pulmonary vasculature can lead to irreversible vascular adjustments and elevated pulmonary vascular resistance. Predictors of mortality in these sufferers include poor functional standing, younger age at presentation or development of symptoms, syncope, supraventricular dysrhythmias, elevated proper atrial pressures, low oxygen saturation (<85%), renal insufficiency, severe proper ventricular dysfunction, and trisomy 21. Heart failure, particularly, right-sided and left-sided failure, is a common complication of each corrected and uncorrected congenital coronary heart illness. Abnormal cardiac autonomic nervous system regulation and altered hemodynamics contribute to the development of heart failure in these sufferers. Approaches for the administration of left ventricular failure are properly documented, and such management must be optimized within the perioperative period. Coagulation and bleeding abnormalities may also be obvious in adults with congenital coronary heart illness. Cyanotic sufferers often have low ranges of circulating vitamin K�dependent clotting elements, issue V, and von Willebrand factor, which finally ends up in an elevated international normalized ratio and a chronic activated partial thromboplastin time. As a result, the elevated whole-blood viscosity with elevated purple cell mass and decreased plasma quantity leads to reduced flow-through within the small arterioles and capillaries. In the perioperative setting, preoperative fasting would possibly exacerbate symptoms of hyperviscosity and improve the danger of cerebrovascular thrombosis; hence, sufficient hydration with intravenous fluids is paramount in these fasting patients, and in some instances, preoperative phlebotomy could be advisable when hematocrit ranges exceed 65%. Coagulation status should even be assessed and doubtlessly corrected in sufferers undergoing moderate or major surgical procedure. In sufferers with Fontan circulation, for instance, central venous stress displays mean pulmonary artery pressure. However, vascular entry could also be difficult because of the presence of scar tissue from prior vessel catheterization. Finally, transesophageal echocardiography may be helpful to monitor intravascular volume standing and ventricular perform. However, intraoperative management should promote tissue oxygen supply by stopping arterial desaturation, maintaining a steadiness between pulmonary and systemic flows, and optimizing hematocrit. Most intravenous brokers depress myocardial contractility and decrease systemic vascular resistance, which may have a deleterious impact on tissue oxygen delivery throughout induction of anesthesia. The use of ketamine has been proven to be helpful in youngsters with congenital coronary heart disease and pulmonary hypertension present process sevoflurane anesthesia as a end result of it maintains ventricular performance and systemic vascular resistance without increasing pulmonary vascular resistance, but it has been related to a rise in pulmonary vascular resistance in adults without congenital coronary heart illness. Intracardiac and systemic-to-pulmonary shunts can present challenges to case management. For example, in sufferers with cyanotic heart illness, ventilation with excessive airway pressures can enhance pulmonary vascular resistance, compromise venous return, and exacerbate right-to-left shunt physiology. Prevention and treatment of pulmonary hypertensive crisis contains hyperventilation (with 1. Inhaled nitric oxide may be helpful for sudden will increase in pulmonary vascular resistance in high-risk sufferers. Regional anesthesia could additionally be an alternate for certain procedures, however a caveat to using spinal and epidural anesthesia is the lower in systemic vascular resistance in patients with unrestrictive intracardiac shunts. The anesthesiologist should also be ready for an elevated intraoperative bleeding danger, such as in sufferers with Fontan circulation with associated liver dysfunction, in addition to potential thrombosis in patients with secondary erythrocytosis. Current suggestions have resulted in a more restrictive use of such prophylaxis. After reviewing the literature for the previous forty years, its professional panel discovered that only a few circumstances of endocarditis may have been prevented by antibiotic prophylaxis. The pointers now emphasize the usage of infective endocarditis prophylaxis in sufferers at high risk, particularly those with prosthetic cardiac supplies.
Diseases - Hemorrhagic thrombocythemia
- Cohen syndrome
- Rhabdomyosarcoma 2
- Osteopetrosis, (generic term)
- Neonatal ovarian cyst
- Goldberg Bull syndrome
Acute will increase in Paco2 are related to increased cerebral blood flow and increased intracranial pressure. Extreme will increase in Paco2 to more than eighty mm Hg could end in central nervous system depression. Carbon Dioxide Elimination the blended venous partial strain of oxygen (Pvo2) and the arterial-venous oxygen difference (Cao2 - Cvo2) replicate the overall adequacy of the oxygen transport system (cardiac output) relative to tissue oxygen extraction. For instance, a lower in cardiac output that occurs within the presence of unchanged tissue oxygen consumption causes Pvo2 to lower and Cao2 - Cvo2 to enhance. These modifications reflect the continued extraction of the identical quantity of oxygen by the tissues throughout a time of decreased tissue blood move. A Pvo2 of less than 30 mm Hg or a Cao2 - Cvo2 larger than 6 mL/dL signifies the necessity to improve cardiac output to facilitate tissue oxygenation. A pulmonary artery catheter permits sampling of blended venous blood, measurement of Pvo2, and calculation of Cvo2. Metabolic acidosis predictably accompanies arterial hypoxemia and insufficient supply of oxygen to tissues. Acidemia attributable to respiratory or metabolic derangements is associated with dysrhythmias and pulmonary hypertension. Alkalemia is often associated with mechanical hyperventilation and diuretic use, which lead to loss of chloride and potassium ions. The incidence of dysrhythmias may be elevated by metabolic or respiratory alkalosis. The presence of alkalemia in sufferers recovering from acute respiratory failure can delay or forestall successful weaning from mechanical air flow because of the compensatory hypoventilation that will occur in an effort to right the pH disturbance. The internet impact is a decrease in Pao2, reflecting dilution of oxygen in blood uncovered to ventilated alveoli with blood containing little oxygen coming from unventilated alveoli. Calculation of the shunt fraction offers a dependable assessment of ventilation/perfusion matching and serves as a useful estimate of the response to various therapeutic interventions during remedy of acute respiratory failure. This degree of right-to-left intrapulmonary shunting displays the passage of pulmonary arterial blood on to the left side of the circulation via the bronchial and thebesian veins. It must be appreciated that determination of the shunt fraction in a affected person respiration lower than one hundred pc oxygen reflects the contribution of ventilation/perfusion mismatching and right-to-left intrapulmonary shunting. Calculation of the shunt fraction from measurements obtained when the affected person breathes one hundred pc oxygen eliminates the contribution of ventilation/perfusion mismatching. The scientific presentation of acute pulmonary thromboembolism ranges from shock or sustained hypotension to gentle dyspnea. Pulmonary embolism could even be asymptomatic and identified by imaging procedures carried out for other purposes. Depending on the scientific presentation, the case fatality rate for acute pulmonary embolism ranges from 1% to 60%. Diagnosis Accurate detection of pulmonary embolism stays difficult, and the differential diagnosis is intensive (Table 9-17). Clinical manifestations of pulmonary embolism are nonspecific, and the diagnosis is commonly tough to establish on clinical grounds alone (Table 9-18). Pleuritic or substernal chest ache, cough, or hemoptysis suggest pulmonary infarction resulting from an embolism near the pleural surface. Other bodily findings include wheezing, fever, rales, a pleural rub, a loud pulmonic element of the second heart sound, a proper ventricular carry, and bulging neck veins. In the presence of a patent foramen ovale or atrial septal defect, paradoxical embolization could happen and interatrial rightto-left shunting of blood may cause extreme hypoxemia. Peaked P waves, atrial fibrillation, and right bundle department block could additionally be current if the pulmonary embolism is sufficiently massive to cause acute cor pulmonale. Transthoracic echocardiography could additionally be particularly helpful in critically unwell sufferers suspected of getting pulmonary embolism and might help establish right ventricular pressure overload in addition to myocardial infarction, aortic dissection, and pericardial tamponade, which may mimic pulmonary embolism. Transesophageal echocardiography could present acute dilation of the right atrium and proper ventricle, pulmonary hypertension, and infrequently even thrombus in the principle pulmonary arteries. Manifestations of pulmonary embolism during anesthesia are nonspecific and often transient. Changes suggestive of pulmonary embolism throughout anesthesia embrace unexplained arterial hypoxemia, hypotension, tachycardia, and bronchospasm. Laboratory testing that aids in the analysis of acute pulmonary embolism consists of the D-dimer test. Troponin levels could additionally be elevated and may symbolize right ventricular myocyte damage attributable to acute right ventricular pressure. It is most useful in detecting clots in the principle, lobar, and segmental pulmonary arteries and is much much less delicate in detecting emboli in smaller blood vessels. Pulmonary arteriography is the gold standard for the diagnosis of pulmonary embolism. It is used when pulmonary embolism must be identified or excluded and different preliminary testing has yielded inconclusive results. The initial evaluation of the medical probability of pulmonary embolism is predicated on clinical judgment. The hypotension brought on by a pulmonary embolism could require remedy with inotropes such as dopamine and dobutamine or a vasoconstrictor such as norepinephrine. Analgesics to treat the ache associated with pulmonary embolism are essential however have to be administered very carefully due to the underlying cardiovascular instability. Management of Anesthesia Management of anesthesia for the surgical therapy of lifethreatening pulmonary embolism is designed to assist important organ operate and to decrease anesthetic-induced myocardial depression. Patients usually arrive within the working room intubated and mechanically ventilated, usually with a high Fio2. Right atrial filling pressure can be a guide to intravenous fluid administration aimed at optimizing right ventricular filling strain and stroke quantity in the presence of a marked improve in proper ventricular afterload. Catecholamines corresponding to dopamine and dobutamine might increase myocardial contractility however have little impact on pulmonary vascular resistance. The phosphodiesterase inhibitors amrinone and milrinone increase myocardial contractility and are wonderful pulmonary artery vasodilators. Induction and maintenance of anesthesia should keep away from any accentuation of arterial hypoxemia, systemic hypotension, or pulmonary hypertension. Removal of embolic fragments from the distal pulmonary artery could also be facilitated by the appliance of optimistic pressure while the surgeon applies suction through the arteriotomy in the primary pulmonary artery. Although the cardiopulmonary status of those patients is perilous before surgical procedure, vital hemodynamic enchancment usually happens postoperatively. Treatment Treatment choices for acute pulmonary embolism include anticoagulation, thrombolytic therapy, inferior vena caval filter placement, and surgical embolectomy. An intravenous bolus of unfractionated heparin (5000 to 10,000 units) adopted by a continuous intravenous infusion ought to be administered immediately to any affected person considered to have a excessive clinical chance of pulmonary embolism. This extended interval of anticoagulation is often accomplished with warfarin in a dosage that maintains a world normalized ratio of two. The use of vena cava filters should be reserved for patients with contraindications to anticoagulant therapy. Retrievable vena cava filters may be an option for patients with presumed time-limited contraindications to anticoagulant therapy or for patients requiring procedures which may be related to each a risk of bleeding and a threat of pulmonary embolism. Hemorrhage is the principal opposed effect of thrombolytic remedy, and so this remedy is contraindicated in sufferers at excessive danger of bleeding. Fat embolism syndrome has also been observed in affiliation with acute pancreatitis, cardiopulmonary bypass, parenteral infusion of lipids, and liposuction. Associated pulmonary dysfunction may be restricted to arterial hypoxemia, which is always present, or it might progress from tachypnea to acute respiratory distress syndrome. Petechiae, particularly over the neck, shoulders, and chest, occur in at least 50% of patients with medical evidence of fat embolism and are thought to be caused by embolic fats rather than by thrombocytopenia or different disorders of coagulation. An increased serum lipase concentration or the presence of lipiduria is suggestive of fat embolism but may happen after trauma in the absence of a fat embolism. Magnetic resonance imaging can present the characteristic cerebral lesions in the course of the acute stage of fats embolism syndrome. The supply of fats producing a fats embolism is most probably disruption of the adipose structure of the bone marrow.
|
|